
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Human immunodeficiency virus (HIV) is a retrovirus that targets the body's CD4+ T lymphocytes, an immune cell involved in the adaptive immune response. Viruses are classified as non-living microbes as they cannot survive independently without a host. Retroviruses are a class of viruses that integrate their viral DNA into the host. We'll take a look at how HIV harnesses this ability to its advantage. The exchange of bodily fluids primarily transmits HIV, and this includes:
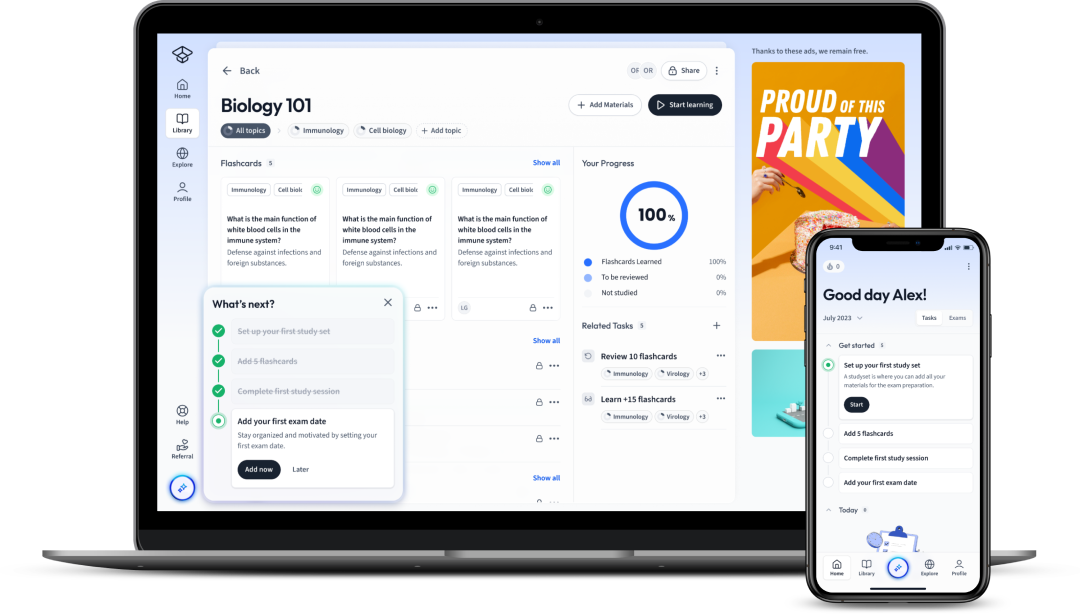
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenHuman immunodeficiency virus (HIV) is a retrovirus that targets the body's CD4+ T lymphocytes, an immune cell involved in the adaptive immune response. Viruses are classified as non-living microbes as they cannot survive independently without a host. Retroviruses are a class of viruses that integrate their viral DNA into the host. We'll take a look at how HIV harnesses this ability to its advantage. The exchange of bodily fluids primarily transmits HIV, and this includes:
HIV-positive patients can develop acquired immunodeficiency syndrome (AIDS) at their most advanced stage, but it is important to note that not all patients do.
Learn more about the importance of CD4+ T lymphocytes in our article T Cell Immunity.
The structure of HIV contains these crucial elements:
HIV is surrounded by a lipid envelope that contains attachment proteins. These attachment proteins facilitate the fusion of HIV to the host cell and are therefore paramount for viral replication. The nucleocapsid (also known as a capsid) surrounds and protects two strands of viral RNA. Within the nucleocapsid, you will also find the reverse transcriptase enzyme. This enzyme catalyses the formation of complementary DNA (cDNA) from RNA. cDNA is important in viral replication as it integrates into the host genome.

As HIV is a virus, it needs a host cell to survive. To establish infection, it binds to a protein called CD4 to facilitate its entry into the host cell. CD4 is a protein found on immune cells, such as helper T lymphocytes, dendritic cells and macrophages. Below, we will discuss the stages of initial attachment to the release of virions.
HIV binds to the CD4 protein found on the surface of immune cells, namely helper T lymphocytes using its viral attachment proteins.
The viral attachment protein gp120 (glycoprotein) binds to CD4.
The lipid envelope of the HIV particle fuses with the cell-surface membrane of the helper T lymphocytes, enabling the entry of the nucleocapsid into the host cell. The host cell environment allows the release of the viral RNA and enzymes into the host cytoplasm. The capsid is degraded.
The viral reverse transcriptase enzyme catalyses the conversion of viral RNA into cDNA.
The newly manufactured viral cDNA is transported into the helper T lymphocyte's nucleus, where it is inserted into the cell's DNA using the viral enzyme integrase.
The integrated viral cDNA is transcribed into mRNA as part of the host genome and leaves the nucleus. The mRNA strands encode the HIV genome and viral proteins.
The mRNA uses the host's protein synthesis organelles to create viral proteins, such as the components needed for the nucleocapsid. These viral components migrate to the host cell's plasma membrane.
Learn more about how proteins are made in our article Protein Synthesis!
The viral particles bud from the host plasma membrane, taking a piece of the plasma membrane with them to create their lipid envelope. The newly released viruses can infect more host cells expressing the CD4 protein.

Acute HIV infection describes the early stages of infection, and clinically, this can manifest as flu-like symptoms after 3-6 weeks as a result of your humoral immune response:
These are very general symptoms that usually persist for 2-6 weeks. After this acute phase, patients undergo an asymptomatic phase where they have entered clinical latency. Patients will initially feel better during this period, but this, unfortunately, does not indicate that the infection has been cleared. Clinical latency occurs when HIV becomes dormant. In other words, the virus resides in your host cells and continues to infect your immune cells.
The T lymphocyte count of patients will drop drastically, and without sufficient T lymphocytes, the adaptive immune response becomes weaker. T lymphocytes are involved in cell-mediated immunity, and with lower cell counts, the production of cytotoxic T lymphocytes and stimulation of B lymphocytes is insufficient. B lymphocytes are involved in humoral immunity, and without sufficient stimulation, antibody production is inhibited.
As the adaptive immune response grows weaker, the patient becomes vulnerable to infection by other pathogens. When the CD4 cell counts decline to the stage where the patient is severely susceptible to opportunistic infection, the patient has developed AIDS.
Opportunistic infections are infections that occur in patients with severely weakened immune systems. HIV patients are most commonly infected with opportunistic pathogens, including Mycobacterium tuberculosis and Salmonella species.
AIDS describes the late stage of HIV infection where a patient's immune system has been severely damaged, leading to susceptibility to opportunistic infections that are unlikely to be developed in those with a normal immune system. Symptoms of AIDS include rapid weight loss, extreme and unexplained tiredness, prolonged swelling of the lymph glands, and pneumonia.
Ultimately, opportunistic infections are the main cause of patient death as they cannot clear the infections.
AIDS is diagnosed by quantifying the number of T lymphocytes in a patient's blood. An uninfected person will typically have between 800 to 1200 T lymphocytes per mm³ of blood. However, patients with AIDS usually have cell counts below 200 per mm³.
A useful diagnostic test for HIV uses the enzyme-linked immunosorbent assay (ELISA). This immunological assay uses antibodies to detect and quantify proteins in a sample. In HIV, ELISA can be used to detect the presence of antibodies against the virus or opportunistic pathogens. The procedure to detect antibodies against HIV is outlined below.
The intensity of the colour change will correspond to the quantity of HIV antibodies present in the sample.
ELISA's are often followed up by another test, such as the Western blot test, before making a positive diagnosis.
Patients are treated using antiretroviral therapy (ART) and this involves the daily combinative administration of HIV drugs that target stages of the viral replicative cycle. Typically, this involves three different drugs, including:
The goal of ART is to suppress viral replication to undetectable levels, reduce transmission and prolong the patient's life. Unfortunately, it is not a cure; it simply controls the virus.
Developing a cure for HIV has proven extremely difficult for researchers due to latent reservoirs of host cells harbouring the virus. These latent reservoirs describe CD4 positive cells that contain the inactive but replication-competent virus. These reservoirs are remarkably long-lived and persist in the blood as they remain undetected by the immune system. These viruses can re-emerge years later and continue to weaken the patient's immune system.
Antibiotics cannot treat HIV as these drugs target bacterial pathogens and are ineffective against viruses.
Antibiotics, such as penicillin and ampicillin, inhibit the synthesis of the bacterial cell wall made of peptidoglycans. Bacteria are formed with pores in their cell walls, and as a result, they cannot withstand the increased pressure of fluids entering into their cells. The bacteria eventually lyse and die.
Viruses have very different structures from bacteria. They do not contain cell walls composed of peptidoglycans. Therefore, antibiotics are ineffective against viruses.
Peptidoglycans are also called murein.
HIV is a retrovirus because it contains the enzyme reverse transcriptase and uses RNA as its genetic material.
HIV infection develops into AIDS when the patient's CD4 T lymphocyte blood count declines below 200 per mm³.
At this stage, the patient is extremely susceptible to opportunistic infections.
HIV stands for the human immunodeficiency virus. It is a retrovirus that binds to CD4 proteins, most commonly found on T lymphocytes.
Antibiotics target bacterial cell walls and are therefore ineffective against viruses. Antibiotics form pores in the peptidoglycan cell wall of bacteria and this leads to lysis. Viruses, however, do not have cell walls.
The first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in