
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Tuberculosis (TB) is currently one of the deadliest infectious diseases caused by bacteria. According to the World Health Organisation (WHO) in 2020, tuberculosis was the second leading cause of death by an infectious disease after COVID-19. Decades after being identified, this disease remains at the centre of a serious public health crisis. It is present in all countries and age groups, however, it is completely curable and preventable with incidence rates falling 2% each year. Ending the tuberculosis epidemic by 2030 is one of the health targets in the Sustainable Development Goals.
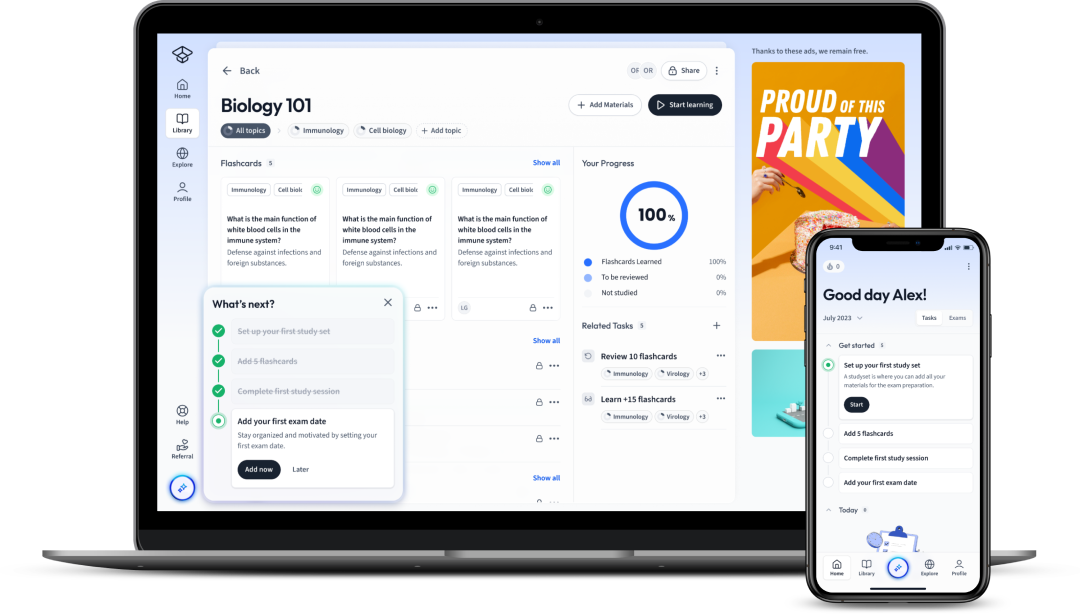
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenTuberculosis (TB) is currently one of the deadliest infectious diseases caused by bacteria. According to the World Health Organisation (WHO) in 2020, tuberculosis was the second leading cause of death by an infectious disease after COVID-19. Decades after being identified, this disease remains at the centre of a serious public health crisis. It is present in all countries and age groups, however, it is completely curable and preventable with incidence rates falling 2% each year. Ending the tuberculosis epidemic by 2030 is one of the health targets in the Sustainable Development Goals.
Tuberculosis (TB) is a bacterial infection which mostly affects the lungs, the primary site of infection. It is an airborne disease. The most well-known tuberculosis symptom is spitting blood when coughing.
Because it affects mostly the lungs, tuberculosis disease is often described as pulmonary tuberculosis.
The two responsible bacterial pathogens for tuberculosis are Mycobacterium tuberculosis and Mycobacterium bovis. These pathogenic bacteria infect human lung tissue living inside human cells but can go on to spread throughout the whole body and infect the lymph nodes, gut, kidney, spine, brain, and even bone tissue.
An estimated 25% of the population is thought to have a tuberculosis infection, but not everyone infected will become sick. The vast majority of people with tuberculosis have a latent tuberculosis infection. This means they harbour tuberculosis bacteria but are not sick and cannot transmit tuberculosis to others. People can have lifetime inactive tuberculosis infection without ever exhibiting symptoms. However, it can develop into tuberculosis disease when the immune system is unsuccessful in fighting off the tuberculosis bacteria.
People with tuberculosis disease have symptoms and can spread the bacteria to others around them, although it usually requires prolonged exposure. Therefore the tuberculosis bacteria incubation period before symptoms onset varies from a few weeks up to several years depending on the ability of the immune system to fight off the bacterial pathogen.
In other words, tuberculosis infection can develop into tuberculosis disease. People with tuberculosis disease can spread the tuberculosis bacteria to others through the air via airborne droplets containing the tuberculosis pathogen.
Tuberculosis can affect anyone and is a leading cause of death in the developing world killing millions of people every year.
Tuberculosis infection is primarily caused by inhaling droplets of liquid in the air containing the tuberculosis bacteria Mycobacterium tuberculosis, i.e. it's an airborne disease. These droplets are released from other infected individuals while coughing or sneezing. Most tuberculosis bacteria enter the body through the respiratory system and go on to attack the lungs, multiplying and causing tuberculosis disease if left unchecked by the immune system.
Tuberculosis infection can also be the result of ingesting meat or milk contaminated with the bacteria Mycobacterium bovis. This less common form of tuberculosis occurs in cattle but can also spread to humans that consume their contaminated meat or milk. This rarely happens in countries where cattle are routinely screened for disease and their milk is pasteurised which kill any present bacteria. However, the infection can occur in countries where unpasteurised milk and undercooked meat are still consumed.
Mycobacterium tuberculosis is an aerobic, acid-fast bacteria species. This means that it requires the presence of oxygen to survive and that it is stained with "acid-fast" stains like the Ziehl-Neelsen stain or fluorescence stains.
Mycobacterium tuberculosis has a particular appearance under the microscope that makes it stand out: it has a waxy coating around its cell membrane due to the presence of mycolic acid. It is this waxy coating that makes it difficult to stain with the traditional Gram staining, so the acid-fast stains are used instead to identify it under the microscope.
 Fig. 2. Mycobacterium tuberculosis under the microscope. Do you notice the waxy appearance of the bacterial colonies?
Fig. 2. Mycobacterium tuberculosis under the microscope. Do you notice the waxy appearance of the bacterial colonies?
The immune system finds attacking Mycobacterium tuberculosis quite difficult. This is because M. tuberculosis is adapted to defend itself from it, especially from macrophages. Macrophages will try to engulf and destroy the bacteria, however, M. tuberculosis fights back.
M. tuberculosis cells can join together to "attack" a single macrophage. The macrophage still engulfs the group of bacteria, but because of the number of bacteria, the macrophage is overpowered and dies. The bacteria then reproduce within the dead macrophage, which is "eaten" by another macrophage with the bacteria still inside. And so the cycle continues, with the bacteria reproducing.
M. tuberculosis also has the ability to remain dormant within the host cells, avoiding the immune system. When the body's conditions are better for M. tuberculosis' survival, the bacteria will activate and start reproducing again.
Tuberculosis is spread when anyone with tuberculosis disease sneezes, spits, or coughs the tuberculosis bacteria from their respiratory system into the surrounding air. If people inhale these particles, they become infected with tuberculosis bacteria.
The tuberculosis bacteria can be suspended by tiny droplets of liquid in the air for several hours.
Once the tuberculosis bacterial pathogen enters the body, the immune system of most healthy people is able to kill the bacteria and prevent tuberculosis disease.
In other cases, the immune system is incapable of killing the bacteria but prevents the Mycobacterium from spreading, causing latent tuberculosis infection. As mentioned before, individuals with latent tuberculosis infection do not have any symptoms and are not infectious to others. If however, the immune system is incapable of fighting the invading pathogen, the tuberculosis bacteria will spread usually first within the lungs and eventually to other parts of the body.
Infected people will then develop active tuberculosis infection or tuberculosis disease and display symptoms within a few weeks or months, infecting others and continuing the transmission cycle. Over the course of a year, people with active tuberculosis infection are thought to infect on average 5-15 other people.
In summary, the development of tuberculosis infection can go three ways:
Individuals with latent tuberculosis infection can also fall ill with tuberculosis disease if their immune system becomes weakened and is no longer capable of containing the dormant tuberculosis Mycobacterium. There are several factors that can contribute to weakening the immune system and to the development of active tuberculosis disease:
alcohol overuse,
smoking,
diabetes,
or even malnutrition
Tuberculosis-infected individuals have, according to the WHO, a 5-10% lifetime risk of developing tuberculosis disease.
HIV infection is one of the most relevant risk factors for tuberculosis illness. People with HIV/AIDS have a compromised immune system that makes them extremely vulnerable to active tuberculosis infection. Tuberculosis is often the first opportunistic infection that HIV-positive patients suffer from.
People living with HIV are multiple times more likely to fall ill with tuberculosis. tuberculosis and HIV make up a very lethal combination, each one contributing to the other’s progressive deterioration. As a result, the HIV pandemic has historically been accompanied by a tuberculosis pandemic.
To learn more about HIV/AIDS and how it attacks our immune system check out our article on HIV.
Active tuberculosis infection can leave individuals severely debilitated if left without treatment. Symptoms of tuberculosis disease include:
Racking cough with sputum and blood
Chest pains
Sweating
Shortness of breath
Fatigue
As part of the immune system’s response against the pathogenic bacteria, people with tuberculosis disease also commonly experience:
The symptoms of tuberculosis disease may start off mild for many months and progressively worsen. The slow onset of tuberculosis symptoms complicates efforts to control the spreading of the disease because it discourages contagious people from seeking treatment early on. People with active tuberculosis infection are at their most contagious stage two to four weeks after becoming infected.
Diagnosis of tuberculosis is very important for controlling the spread of the disease. Tuberculosis infection, including latent infection, can be confirmed through the Mantoux tuberculin skin test (TST) or blood tests.
The Mantoux tuberculin skin test consists of injecting tuberculin (a mix of antigens from the bacteria that cause tuberculosis) into the forearm. After some time, the swelling around the area of the injection is measured. A positive or negative diagnosis depends on the size of the swelling.
Tuberculosis disease usually requires additional diagnosis. WHO guidelines recommend tuberculosis disease diagnosis be done using rapid molecular diagnostic assays that rely on nucleic acid amplification, such as polymerase chain reaction (PCR) tests. These tests confirm tuberculosis disease by detecting the presence of the tuberculosis bacteria’s genetic material in a clinical sample.
Other methods of tuberculosis disease diagnosis involve:
Patients with active tuberculosis infection either suspected or confirmed should be ideally isolated from others during their most infectious stage to prevent further contagion.
Despite killing millions, tuberculosis is a treatable and curable disease. As with most other bacterial infections, treatment involves the use of antibiotics that kills the tuberculosis bacteria. Active tuberculosis infection is treated with a multi-month regimen of several antibiotic drugs like isoniazid and rifampicin. This combination of drug therapeutics usually cures up to 95% of all tuberculosis patients.
One of the reasons there was a resurgence of tuberculosis disease in the last decades across the world was the added difficulty in providing effective treatment. Overuse and inappropriate use of antibiotics have led many bacteria to become resistant to these drugs. Like all other organisms, bacteria mutate and find new ways to evade the antibiotic’s function. Tuberculosis therapeutics is no exception, with the appearance of Mycobacterium-resistant strains to first-line anti-tuberculosis drugs.
Multidrug-resistant forms of tuberculosis (MDR-TB) and even extensively drug-resistant forms of tuberculosis (XDR-TB) have emerged as serious public health threats. The emergence of drug-resistant forms of tuberculosis bacteria has been partly fuelled by inappropriate usage of tuberculosis antibiotics including incorrect prescriptions, poor-quality drugs and especially patients stopping their treatment before completion.
Tuberculosis treatment can last anywhere from at least 6 to 9 months or longer and must be completed in full even if the patient begins to feel better before finishing their treatment. A long treatment time is required to ensure all bacteria are killed.
Stressing the importance of patients completing their treatment regimens is essential to successfully reducing tuberculosis incidence. Prematurely stopping the antibiotic treatment gives any remaining living bacteria a chance to mutate and evade the antibiotic action later. This originates drug-resistant strains that go on to infect others, further complicating the effort to stop tuberculosis outbreaks.
Treatment for resistant strains requires the use of new antibiotics and treatments, often more expensive and less potent resulting in even longer multi-year treatment regimens.
To learn more about how antimicrobial drugs kill bacteria and the emergence of antibiotic resistance, check out our article on Antibiotics!
Nevertheless, according to the WHO, since the year 2000, tuberculosis treatment has saved upwards of 60 million people! Without access to these treatments, it’s estimated that almost half of HIV-negative people with tuberculosis disease and almost all HIV-positive people with tuberculosis disease would die.
General tuberculosis prevention efforts can be very important in reducing tuberculosis incidence. General strategies like contact tracing, implementing rapid tuberculosis diagnosis, and programs that follow up with tuberculosis patients and encourage them to continue their treatments are all important to tackle tuberculosis disease.
Another possible preventive measure to tackle tuberculosis disease is the tuberculosis vaccine, BCG. BCG is a moderately effective vaccine, protecting up to 80% of children who receive it. As such, BCG is mainly used in children or young adults considered to be at risk.
At-risk groups can include those living in areas with high tuberculosis incidence or with family members that become ill with tuberculosis disease. The BCG vaccine is typically not given to people over the age of 35 as its efficacy significantly decreases with higher age groups.
The bacterial pathogen Mycobacterium tuberculosis or Mycobacterium bovis.
Tuberculosis spreads through the air via airborne droplets containing tuberculosis germs. These droplets are released into the air when someone with tuberculosis disease sneezes or coughs them up. Any person close enough to inhale them will become infected with tuberculosis.
A bacterial infectious disease.
Racking cough, fever, weight loss, sweating, chest pains, shortness of breath.
BCG is a live attenuated vaccine.
Flashcards in Tuberculosis15
Start learningTB is a viral infectious disease. True or false?
False
What organ do the TB bacteria primarily target?
Lungs
What is the name of the TB vaccine?
BCG
What is the main method of transmission of tuberculosis?
Airborne droplets containing TB germs.
All people infected with TB bacteria have TB disease. True or false?
False
What kind of drug therapeutics are used to treat TB?
Antibiotics

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in