
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Delving into the pressing issue of bacterial resistance to antibiotics, this comprehensive article unfolds this complex phenomenon, providing a clear understanding of the subject. You'll explore the reasons behind bacterial resistance, the mechanisms by which this resistance arises, including horizontal gene transfer, and learn about bacteria that have yet to acquire resistance. You'll also gain valuable insights into preventative strategies, the importance of proper antibiotic usage, and crucial public health measures. Undoubtedly essential in today's medical landscape, this article shines a spotlight on confronting and countering bacterial resistance to antibiotics.
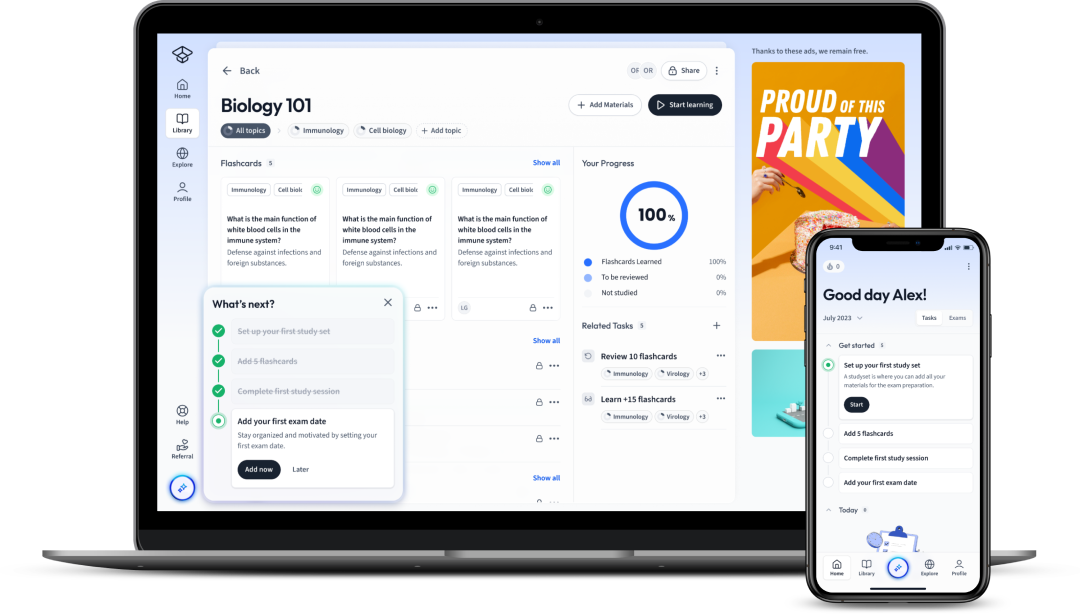
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDelving into the pressing issue of bacterial resistance to antibiotics, this comprehensive article unfolds this complex phenomenon, providing a clear understanding of the subject. You'll explore the reasons behind bacterial resistance, the mechanisms by which this resistance arises, including horizontal gene transfer, and learn about bacteria that have yet to acquire resistance. You'll also gain valuable insights into preventative strategies, the importance of proper antibiotic usage, and crucial public health measures. Undoubtedly essential in today's medical landscape, this article shines a spotlight on confronting and countering bacterial resistance to antibiotics.
Bacterial resistance to antibiotics, a fascinating and significant subject of microbiology, is a phenomenon that occurs when bacteria mutate or acquire genes from other bacteria, enabling them to survive exposure to the antibiotics designed to kill them. A deep understanding of this subject is crucial to tackling growing issues related to antibiotic resistance worldwide.
This topic inititates an exploration into why some bacteria aren't eliminated by antibiotics, contrary to what one might expect. The development of bacterial resistance to antibiotics is often due to genetic changes that occur over generations within bacterial populations.
Bacterial resistance can be defined as the ability of bacteria to withstand the effects of an antibiotic they were once susceptible to.
All bacteria have the inherent ability to resist antibiotics due to mutation and the uptake and transfer of resistance genes from one bacterium to another.
In simple terms, when a bacterium is exposed to an antibiotic, if it has a mutation that allows it to survive, it will then replicate itself, and soon most of the bacteria will be resistant to that antibiotic. This can be represented by the formula \( R_t = R_0(1+ r)^t \), where \(R_t\) is the final amount of bacteria, \(R_0\) is the initial amount, \(r\) is the growth rate, and \(t\) is time.This concept of survival of the fittest, laid out by Charles Darwin, is as applicable to bacteria as it is to all living beings.
With the prevailing misuse and overuse of antibiotics, the terrifying escalation of bacterial resistance has rapidly evolved. Unlike what occurs in multicellular organisms, mutations in bacteria can directly create new traits since each bacterium carries a complete copy of its genome. This can lead to the speedy propagation of antibiotic-resistant genes between individual cells, leading to a substantial obstacle in medicine – the inability to efficiently treat bacterial infections.
Although the threat of antibiotic resistance is genuine and growing, it's noteworthy that many bacterial infections are still effectively treated by antibiotics. These bacteria have not yet developed substantial resistance or have mechanisms of virulence that can be blocked by specific antibiotics.
It's essential to remember that even for these infections, the correct usage of antibiotics plays a critical role in preventing potential bacterial resistance.
While we're focused on bacterial resistance, it's crucial to remember that many bacterial species readily respond to antibiotics.
For instance, Bacillus anthracis, the bacterium that causes Anthrax can be efficiently treated with antibiotics such as Ciprofloxacin. Among others, the bacteria causing Lyme disease, Borrelia burgdorferi, is effectively eliminated with Doxycycline or Amoxicillin treatment.
In conclusion, while bacterial resistance to antibiotics continues to present a major challenge in microbiology and medicine, it's important to have a nuanced understanding of the topic, including both the pitfalls and the areas where we continue to have success with antibiotic treatment. Crucially, responsible use of antibiotics will play a significant role in battling the rise of antibiotic resistance.
Bacterial resistance to antibiotics is primarily driven by genetic changes within bacterial populations, which can happen for several reasons. The key causes to delve into include overuse and misuse of antibiotics, alongside the natural propensity of bacteria for mutation and evolution. The significance of various mechanisms such as horizontal gene transfer also needs to be investigated.
There are multiple factors contributing to antibiotic resistance, and it's crucial to understand these to tackle the issue at its foundation. It all stems from the natural genetic variability in bacterial communities. However, certain practices, such as the overuse and misuse of antibiotics, particularly accelerate this process.
When antibiotics are used excessively or incorrectly, bacteria are exposed to selective pressure which encourages the survival and replication of resistant strains. This upset to the natural balance of microbial communities can even provoke resistance in previously susceptible organisms. Here, high genetic variability gives bacteria a greater chance of developing resistance. Furthermore, bacteria can transfer these resistance genes to subsequent generations or even to other bacteria, thus propagating resistance.
Other factors that contribute to antibiotic resistance include inadequate diagnosis, lack of access to quality healthcare, poor hygiene and sanitation practices, and inappropriate antibiotic use in agriculture.
The overuse and misuse of antibiotics undoubtedly acts as a catalyst for antibiotic resistance. When these powerful drugs are used unnecessarily (for conditions they can't treat, such as viral infections) or incorrectly (not following the prescribed dosage or duration), they provide bacteria the perfect environment to develop and spread resistance.
If a course of antibiotics is not completed, it's likely that some bacteria will survive, learning how to defend themselves against that particular drug. These resistant bacteria can then multiply, leading to a larger population of antibiotic-resistant bacteria. This can be represented by the formula \( R_t = R_0(1+ r)^t \), where \(R_t\) is the final number of bacteria, \(R_0\) is the initial number, \(r\) is the growth rate, and \(t\) is time. This formula broadly illustrates the growth of bacterial populations subjected to incomplete antibiotic treatments.
Moreover, overuse of antibiotics in animals and agriculture can lead to resistant bacteria in the food chain, contributing to the overall problem of resistance.
Understanding the exact mechanisms behind bacterial resistance to antibiotics is an essential part of microbiology. Below, let's delve into how bacteria adapt and respond to these therapeutic threats on a molecular level.
As a basic survival strategy, bacteria can mutate or modify their genes to withstand the effects of antibiotics. Through these changes, bacteria can reduce the effectiveness of antibiotics by:
However, the most crucial and fascinating mechanism is horizontal gene transfer where resistance genes are shared amongst bacteria.
One of the key factors in bacterial resistance is the ability of bacteria to transfer genetic information horizontally (between individual cells) rather than vertically (from parent to offspring). Horizontal gene transfer can happen through three main methods:
| Transformation | The uptake of genetic material from the environment |
| Transduction | The transfer of genetic material through bacterial viruses |
| Conjugation | The direct transfer of genetic material from one bacterium to another |
This process significantly accelerates the spread of antibiotic resistance and complicates attempts to control the problem. Hence, any solution to the global issue of antibiotic resistance must consider the implications of horizontal gene transfer.
Indeed, bacterial resistance to antibiotics is a significant and challenging issue that needs to be addressed urgently. However, it's not an insurmountable problem. With focused efforts in the right direction, such as leveraging preventive strategies and reinforcing public health measures, we can effectively counter this escalating threat.
Preventing bacterial resistance to antibiotics necessitates decisive action on multiple fronts. First and foremost, it's essential to reassess and optimise the use of antibiotics. Widespread misuse and overuse of these drugs are key drivers in the evolution of bacterial resistance, thus stringent measures to monitor and control their application are pivotal. Simultaneously, research into new and effective antibiotics needs to be ramped up, to keep pace with evolving bacterial threats.
Further, the use of antibiotics in agriculture and animal breeding also requires careful reevaluation. A substantial amount of antibiotics is employed in these sectors, often leading to drug-resistant bacteria that can potentially transfer to humans.
Let's dive deeper into these factors:
The importance of proper usage of antibiotics cannot be overstated in maintaining their efficacy against bacterial infections. Misuse of these powerful drugs can not only lead to treatment failure but also, more alarmingly, foster the emergence of antibiotic-resistant bacteria.
Appropriate usage of antibiotics involves several critical considerations:
Public health measures play a critical role in the battle against bacterial resistance to antibiotics. In the broader perspective, these encompass initiatives like vaccination, maintenance of proper hygiene, and education about antibiotic resistance. All these can significantly impact the reduction in antibiotic resistance.
Each of these initiatives offers substantial benefits:
Vaccination and hygiene are two pivotal cogs in the machinery of public health tasked with countering antibiotic resistance. Vaccines work proactively to prevent bacterial infections, reducing the need for post-infective antibiotic application. Hence, immunisation is a highly effective way to slow the development of antibiotic resistance.
Moreover, maintaining good hygiene practices can prevent the spread of bacterial infections, thus limiting the necessity for antibiotic usage. This encompasses practices such as hand hygiene, safe food handling, and sanitation. It's vital to remember many antibiotic-resistant bacteria can spread through contaminated food, water, or contact with infected individuals or surfaces.
These two practices combined with public education campaigns form an excellent triad to tackle antibiotic resistance proactively.
Flashcards in Bacterial Resistance to Antibiotics39
Start learningHow can bacterial resistance to antibiotics be defined?
Bacterial resistance is the ability of bacteria to withstand the effects of an antibiotic which they were once susceptible to.
What causes bacterial resistance to antibiotics?
Resistance happens when bacteria mutate or acquire resistance genes from other bacteria, allowing them to survive exposure to antibiotics.
What is one bacterial infection that is still effectively treated by antibiotics?
Strep throat, caused by the bacteria Streptococcus pyogenes, is still effectively treated by antibiotics.
What is a preventive measure against potential bacterial resistance?
Correct usage of antibiotics plays a critical role in preventing potential bacterial resistance.
What are some of the causes of antibiotic resistance?
The causes include genetic changes in bacteria due to exposure to antibiotics, overuse and misuse of antibiotics, poor hygiene, inadequate diagnosis, and inappropriate antibiotic use in agriculture.
What happens when antibiotics are used excessively or incorrectly?
When antibiotics are misused, bacteria are exposed to selective pressure which encourages the survival and propagation of resistant strains. Incomplete courses can allow surviving bacteria to learn how to defend against that antibiotic.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in