
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Discover the indispensable world of antibiotics as you delve into this comprehensive guide on various classes of antibiotics. This informative piece unravels the definition and history of antibiotics, offers a deep understanding of different antibiotic classes, their mechanisms of action, and unique characteristics. You'll explore a thorough list of antibiotic classes including broad-spectrum, narrow-spectrum, and the prominent Penicillin class. Additionally, this article brings to light the practical applications of these classes in treating communicable diseases and their impact, including the serious issue of antibiotic resistance. As a microbiology enthusiast or professional, enlighten yourself about making the right antibiotic choice for preventing communicable diseases.
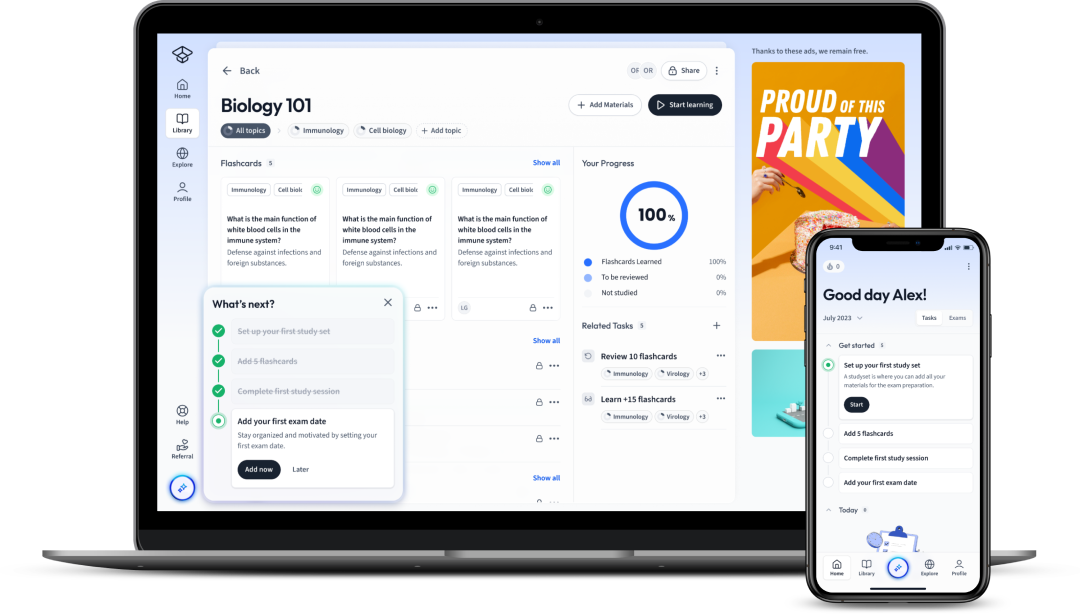
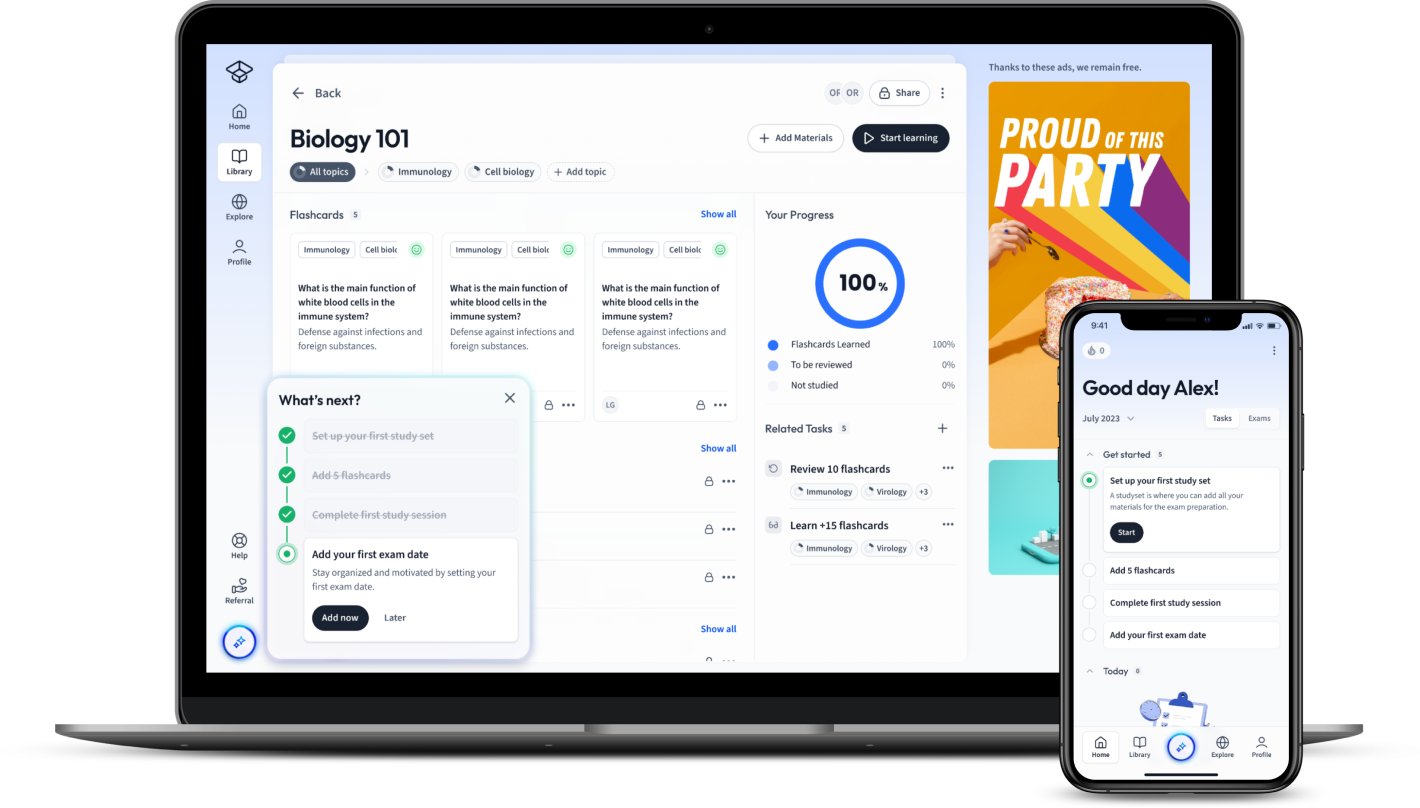
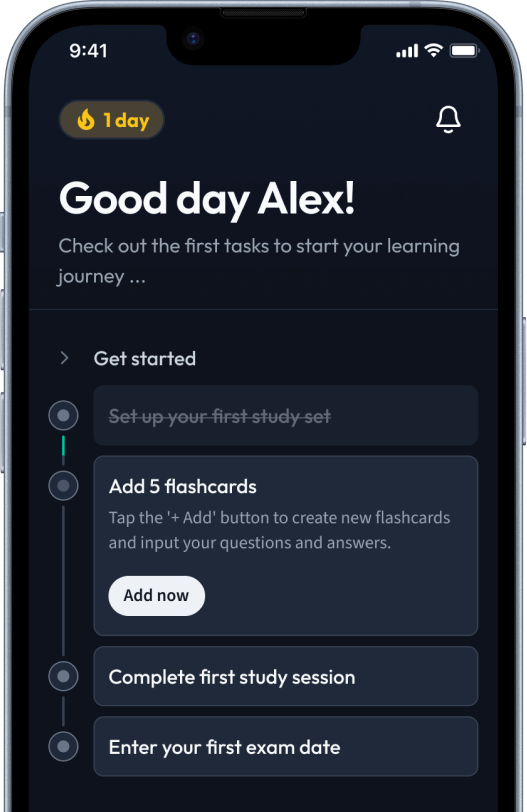
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDiscover the indispensable world of antibiotics as you delve into this comprehensive guide on various classes of antibiotics. This informative piece unravels the definition and history of antibiotics, offers a deep understanding of different antibiotic classes, their mechanisms of action, and unique characteristics. You'll explore a thorough list of antibiotic classes including broad-spectrum, narrow-spectrum, and the prominent Penicillin class. Additionally, this article brings to light the practical applications of these classes in treating communicable diseases and their impact, including the serious issue of antibiotic resistance. As a microbiology enthusiast or professional, enlighten yourself about making the right antibiotic choice for preventing communicable diseases.
Delve into the fascinating world of antibiotics - the tiny powerhouses countering harmful microorganisms. As a keystone topic in Microbiology, understanding the various Classes of Antibiotics equips you with the knowledge to discern their unique uses, modes of action, and significant bacterial resistance issues.
Antibiotics are a type of antimicrobial drugs used in the treatment of bacterial infections. They work in one of two ways: by killing bacteria or inhibiting their growth.
The 'birth' of Antibiotics can be traced back to 1928 with Alexander Fleming's serendipitous discovery of Penicillin, thanks to a rogue mould named Penicillium Notatum obstructing a culture of Staphylococcus bacteria.
This event heralded a new era in the medical field with antibiotics becoming a crucial tool against infectious diseases. Since then, multiple classes have been derived, each having its own specific functions and target bacteria.
For instance, based on their chemical structure, these classes include Penicillins, Cephalosporins, Macrolides, and Quinolones, each targeting different types of bacteria and possessing distinct modes of action.
Aside from natural production, some antibiotics are semisynthetic - modified versions of naturally occurring substances. Others are entirely synthetic, designed and created within the laboratory.
Understanding the Classes of Antibiotics is vital in the field of Microbiology. Their study offers insights into bacterial physiology - the very targets they seek to combat. By deciphering the mechanisms of action for different antibiotics, you expose vulnerabilities in the bacterial cell processes, promoting the discovery of new antibacterial strategies.
Knowledge about the antibacterial class helps to choose the right drug for particular bacterial infections
Consider Streptococcus Pneumoniae. Having insight into the organism's susceptibility to Penicillin class of antibiotics, you might choose this to effectively hinder the cell wall synthesis of the bacteria, weakening and eliminating the infection
Moreover, studying the classes of antibiotics allows us to explore trends and issues in bacterial resistance. Noting how different classes may incite resistance differently underscores the importance of prudent antibiotic use, steering us towards optimal patient outcomes and public health initiatives.
For instance, overuse of a Class like Quinolones can lead to quickly developing resistance. The bacteria alter the very enzymes targeted by the antibiotic, rendering the drug ineffective.
Last but not least, you gain a comprehensive view of the pharmacokinetics, toxicity profiles, and contraindications associated with each class - absolutely vital when considering patient safety and drug efficacy.
Delving deeper into the classes of Antibiotics, let's peep into their varied mechanisms of action and examples. Gaining insights into each class's unique actions further enhances your understanding of how these compounds wage 'war' against bacteria.
Different classes of antibiotics possess varied mechanisms of action. Generally, these can be summarised into four primary actions:
| Class | Mechanism of Action |
| Penicillins | Inhibition of Cell Wall Synthesis |
| Polymyxins | Disruption of Cell Membrane Function |
| Macrolides | Inhibition of Protein Synthesis |
| Quinolones | Interference with Nucleic Acid Synthesis |
Each class of antibiotics has representatives that best illustrate the action mode unique to the class. To understand this, let's discuss some specific examples.
Classes of Antibiotics are determined by various distinguishing factors, each contributing to the drug's unique antibacterial activity and properties. The decisive factors include:
The term 'Spectrum of activity' refers to the range of bacteria that an antibiotic can act upon.
Peeling the layers back, you realise that several factors impact the differentiation of antibiotic classes.
The chemical structure hugely influences the class of an antibiotic. For instance, Penicillins are characterised by the presence of a beta-lactam ring in their structure. You'll find Cephalosporins also possess this ring although have a different side chain, distinguishing them from the Penicillins.
Next, the mechanism of action plays a vital role in class determination; the approach by which antibiotics engage with bacteria differs uniquely across classes. As such, we have classes that inhibit cell wall synthesis, disrupt cell membranes, hinder protein synthesis, or obstruct nucleic acid synthesis.
Differences in spectrum of activity also help categorise antibiotics. For instance, you'll find that the Macrolides, with broad-spectrum activity, can inhibit a wide range of Gram-positive and some Gram-negative bacteria, unlike the narrow spectrum Penicillins that primarily target Gram-positive bacteria.
Finally, the bacteriostatic or bactericidal nature of the antibiotics is also a determinant factor for the classes. As an example, Aminoglycosides, like Streptomycin, are bactericidal and kill bacteria primarily while Tetracyclines are typically bacteriostatic inhibiting bacterial growth.
Antibiotics are separated into wide-ranging classes depending on their chemical structure, mechanism of action, spectrum of activity, and whether they are bactericidal or bacteriostatic. This section discusses some of the highly prevalent Classes of Antibiotics, from broad-spectrum to narrow-spectrum and specific classes like Penicillins.
Broad-spectrum antibiotics are effective against a wide range of bacteria, both Gram-positive and Gram-negative. Though they are important tools in managing various infections, it's crucial to recognise their potential impact on normal flora and the risk of developing resistance.
Sharing some examples:
It's useful to note that because of their broad-spectrum activity, these antibiotics can disrupt the normal flora, potentially leading to secondary infections such as Clostridium difficile infection. Additionally, overuse can enhance the risk of antibiotic resistance.
Narrow-spectrum antibiotics, as their name implies, have a more focused range of activity compared to broad-spectrum agents. They are primarily effective against specific types of bacteria.
These antibiotics reduce the chance of disrupting normal flora compared to broad-spectrum antibiotics. Moreover, careful use reduces the chances of resistance development.
The Penicillin class of antibiotics, derived from fungi of the genus Penicillium, was the first set of antibiotics discovered. These agents work primarily by inhibiting cell wall synthesis specifically via the interruption of peptidoglycan cross-linking.
Bear in mind that the effectiveness of penicillin antibiotics can be compromised by bacterial production of \(\beta\)-lactamase enzymes, which inactivate the antibiotic by cleaving the \(\beta\)-lactam ring integral to its structure. Subsequently, clinicians frequently use inhibitors like Clavulanic acid alongside Penicillin antibiotics to combat this resistance mechanism.
Note that allergies are a critical concern with Penicillin use, as some patients may experience reactions ranging from mild rashes to severe anaphylactic responses. Therefore, allergy history is a crucial consideration when prescribing this class of antibiotics.
The significance of antibiotics extends beyond their diversity and structural differences. The practical applications of these classes of antibiotics place their value in the treatment of various bacterial infections and communicable diseases. Furthermore, they play pivotal roles in procedures like surgery, providing prophylaxis against potential post-operative infections. This section elucidates more on such use-cases.
Each class of antibiotics serves distinct roles in managing various bacterial infections. These antibiotics target different bacterial species and systems, thereby prescribing them in-line with the causative bacterial agent of an infection.
Broad-spectrum antibiotics, such as Quinolones and Macrolides, are usually the first-line treatment for severe and undiagnosed infections since they cover a wide range of bacteria. Their wide coverage enables doctors to initiate therapy whilst the exact causative agent is still unidentified.
As they become aware of the specific bacteria causing the infection (after laboratory testing), they may switch to a narrow-spectrum antibiotic to reduce possible risks of antibiotic resistance and disruption of normal flora.
Penicillins and cephalosporins are among the most commonly prescribed classes of antibiotics due to their broad spectrum of activity and low toxicity. They are used for various infections, including skin infections, respiratory tract infections, and urinary tract infections.
In contrast, aminoglycosides are often reserved for severe infections caused by Gram-negative bacteria due to their potential side effects, including hearing loss and kidney damage.
Vancomycin, a glycopeptide antibiotic, is a drug of choice for MRSA (Methicillin-resistant Staphylococcus aureus) infections and serious infections caused by other Gram-positive bacteria.
The Penicillin class of antibiotics, given their low toxicity and broad applicability, finds widespread use in treating a variety of bacterial infections. For instance, Penicillin G and V, being active against Gram-positive organisms, are pivotal in combating Streptococcal infections (including Streptococcal pharyngitis and Pneumococcal pneumonia) and Syphilis. Additionally, this class features Penicillinase-resistant Penicillins (like Dicloxacillin), which are employed in tackling infections caused by Penicillinase-producing Staphylococci.
Then there are Aminopenicillins, such as Ampicillin and Amoxicillin, which demonstrate increased activity against Gram-negative bacteria, extending their use to infections like urinary tract infections and Haemophilus influenzae respiratory tract infections. The addition of a \(\beta\)-lactamase inhibitor (like Clavulanic acid) increases the antibiotic's resistance to bacterial defences, thus broadening the spectrum to cover \(\beta\)-lactamase producing bacteria.
Importantly, the role of Penicillins is prominent in prophylactic (preventive) therapy. Procedures such as dental work or surgical incisions in patients with certain heart conditions could expose the bloodstream to bacterial infection, leading to a condition known as infective endocarditis - a serious infection of the heart chambers and valves. Application of antibiotics belonging to the Penicillin class plays a significant role in averting such infections.
When dealing with communicable diseases, antibiotics exert significant therapeutic and controlling effects. Certain diseases, like Tuberculosis, Syphilis, and Gonorrhea, caused by bacterial pathogens, have antibiotics as the cornerstone of their treatment strategies. Importantly, the judicious use of these antibiotics also helps contain the spread of these diseases.
Tuberculosis remains one of the most devastating communicable diseases worldwide. A combination of antibiotics such as Rifampicin, Isoniazid, Pyrazinamide, and Ethambutol over a long duration remains key to managing this disease caused by Mycobacterium tuberculosis.
Meanwhile, Syphilis, primarily a sexually transmitted infection caused by Treponema pallidum, finds Penicillin G as the antibiotic of choice. Even in late-stage cases of this disease, high doses of this drug showcase great effectiveness.
In light of the escalating cases of Gonorrhea, caused by Neisseria gonorrhoeae, the current treatment involves a dual-antibiotic therapy. Here, an injection of the Cephalosporin antibiotic, Ceftriaxone, is combined with Azithromycin oral administration. This combats the increasing antibiotic resistance and successfully manages the infection.
It’s imperative to realise the role of antibiotics in mitigating these and many other communicable diseases, thus highlighting their role in public health. However, the increasing resistance to these drugs calls for more careful and informed use and stimulates the need for continuous research and development of new antimicrobial agents.
Antibiotics, as key weapons in our medicinal arsenal against bacterial infections, play a decisive role in curbing communicable diseases. An appropriate choice aligns with the nature and severity of the infection, susceptibility patterns of the causative bacteria, and patient-specific factors. However, the influence of antibiotic choice on the broader landscape of communicable diseases cannot be understated. The emergence of antibiotic resistance and the inability to prevent disease spread are some significant challenges revealing this impact.
Over the decades, antibiotics have radically revolutionised the management of bacterial infections. However, their unwarranted use and misuse, driven by insubstantial diagnostic measures or non-adherence to treatment regimens, have fueled a global health crisis - antibiotic resistance.
It happens when bacteria adapt to the drugs meant to destroy them, rendering therapeutic interventions ineffective. This phenomenon has severe implications for the control of communicable diseases as it reduces the efficacy of antibiotics, leading to prolonged illness, increased mortality, and the potential for disease spread.
Consider the case of Tuberculosis. Multidrug-resistant Tuberculosis (MDR-TB), resistant to both Rifampicin and Isoniazid, and extensively drug-resistant Tuberculosis (XDR-TB), further resistant to any fluoroquinolone and at least one of the three injectable second-line drugs, pose critical threats to Tuberculosis control. The rise of these forms of drug resistance has made disease management challenging and substantially reduced treatment success rates.
Methicillin-resistant Staphylococcus aureus (MRSA), resistant to most beta-lactam antibiotics, including penicillins and cephalosporins, has increasingly become a significant cause of hospital-acquired and community-acquired infections. Its emergence complicates treatment, calling for the use of reserved antibiotics like Vancomycin and Linezolid.
Situations like these highlight the urgent need for careful antibiotic choices, new drug development, and more significant efforts towards global antibiotic stewardship to keep resistance in check.
The association between the choice of antibiotic classes and the development of resistance is complex. Widespread use or misuse of a certain class leads to increased selection pressure on bacteria, driving mutations aiding survival against that antibiotic class, and subsequent proliferation of these resistant strains.
Notice that the use of broad-spectrum antibiotics often exerts greater selective pressure. A broad-spectrum antibiotic, due to its activity against a wide range of bacteria, alters the bacterial flora extensively. This can bestow an environment conducive for the growth of drug-resistant strains. Hence, using these antibiotics judiciously becomes crucial to avoid antibiotic resistance.
The Penicillins represent a class of antibiotics where the influence of bacterial resistance is significantly noted. The production of beta-lactamases by bacteria, enzymes that destroy the effective beta-lactam ring in Penicillins, is a common mechanism of resistance. This has led to the development of newer Penicillins, displaying beta-lactamase resistance, such as Methicillin and Oxacillin, and the use of beta-lactamase inhibitors such as Clavulanate with drugs like Amoxicillin.
The production of modified drug targets, efflux pumps (proteins expelling the drug out of the bacteria), and antibiotic modifying enzymes are other mechanisms deployed by bacteria against varying classes of antibiotics.
The choice of an antibiotic class significantly influences the ability to prevent the spread of communicable diseases. Preventive strategies, involving prophylactic antibiotic use and timely treatment of infections, hinge on the selection of the most appropriate antibiotic.
Using antibiotics to prevent bacterial infections (prophylaxis) is a common practice in situations where the risk of infection is high, such as surgeries or dental procedures in people with specific heart conditions. The Penicillins, due to their excellent safety profile and effectiveness against common surgical pathogens, are often selected for prophylaxis. However, the patient's allergy history and the regional susceptibility patterns of organisms play a role in deciding the right antibiotic class.
The date provided by culture and sensitivity tests helps select the most effective class of antibiotics against the identified bacteria, ensuring quick recoveries and decreasing the potential for disease transmission. Empiric therapy, involving the initial use of broad-spectrum antibiotics to cover the most likely infectious agents, gradually switches to a targeted narrow-spectrum antibiotic once the culture results are available. This cautious approach aids in controlling diseases spread and curbing antibiotic resistance.
It is vital to recognise the profound implications of antibiotic choice for communicable diseases. Choosing the right antibiotic and class, adapted to clinical needs and guided by the principles of antibiotic stewardship, will be decisive in winning the battle against communicable diseases and antibiotic resistance.
Flashcards in Classes of Antibiotics57
Start learningWhat are the two ways by which antibiotics work in the body?
Antibiotics work either by killing bacteria or inhibiting their growth.
Why is studying classes of antibiotics important in microbiology?
Studying classes of antibiotics helps understand bacterial physiology, enables the right antibiotic selection for specific bacterial infections, allows exploring trends in bacterial resistance, and provides a comprehensive view of the pharmacokinetics, toxicity profiles and contraindications of each class.
What was the first type of antibiotic discovered and when was it discovered?
The first type of antibiotic, Penicillin, was discovered in 1928 by Alexander Fleming.
What are the four primary mechanisms of action of antibiotics?
The four primary mechanisms of antibiotics are: inhibition of cell wall synthesis, disruption of cell membrane function, inhibition of protein synthesis, and interference with nucleic acid synthesis.
What determines the class of an antibiotic?
The class of an antibiotic is determined by factors like its chemical structure, spectrum of activity, whether it's bactericidal or bacteriostatic, and its mode of action.
What are the examples of different classes of antibiotics and their mechanisms?
Examples are Penicillins (Inhibition of cell wall synthesis), Polymyxins (Disruption of cell membrane function), Macrolides (Inhibition of protein synthesis), and Quinolones (Interference with nucleic acid synthesis).
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
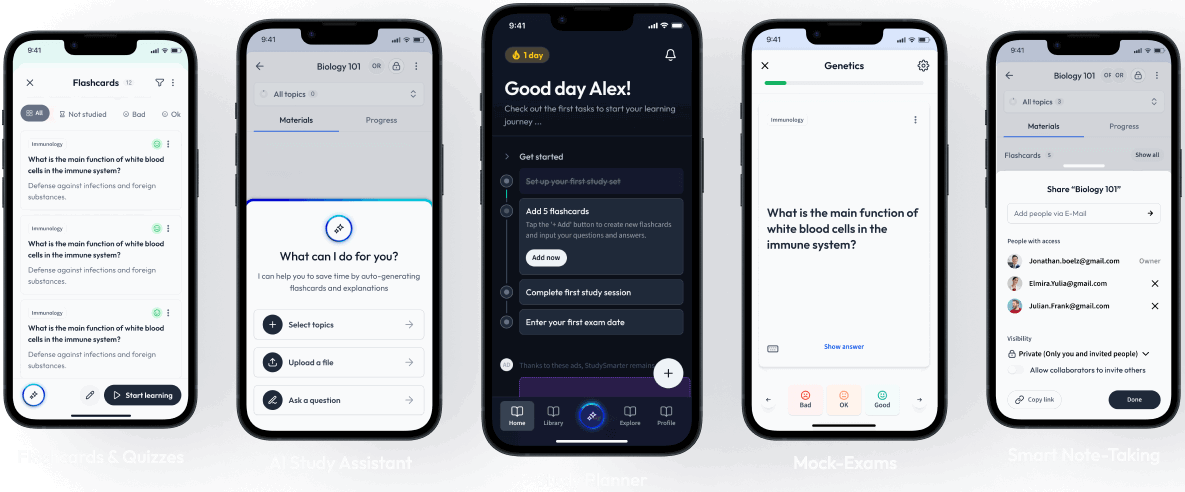
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in