
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
A drug is any substance that, when taken into the body, modifies or impacts the chemical reactions which underpin body metabolism. While you may immediately jump to marijuana or cocaine as examples of drugs, many things all around you are technically drugs. These include alcohol and caffeine, which are regularly consumed by adults worldwide. Also included in the use of drugs as a catch-all term are the medicines used throughout the world to treat medical conditions every day. It's this type of drug people are generally referring to when using the term drug development, and it's what we will be discussing in this article.
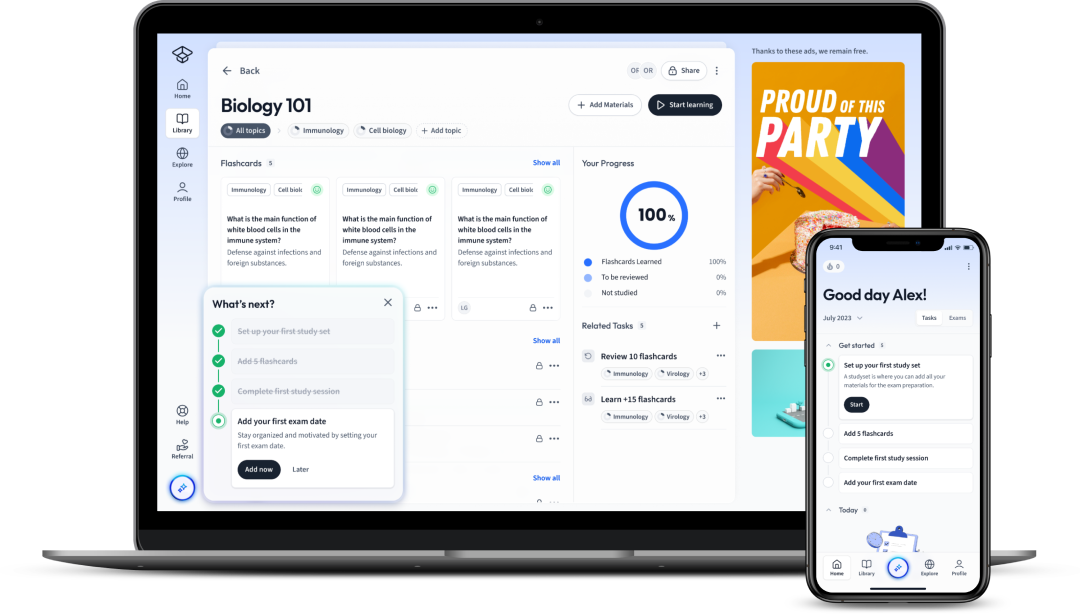
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenA drug is any substance that, when taken into the body, modifies or impacts the chemical reactions which underpin body metabolism. While you may immediately jump to marijuana or cocaine as examples of drugs, many things all around you are technically drugs. These include alcohol and caffeine, which are regularly consumed by adults worldwide. Also included in the use of drugs as a catch-all term are the medicines used throughout the world to treat medical conditions every day. It's this type of drug people are generally referring to when using the term drug development, and it's what we will be discussing in this article.
A drug is any substance that, when introduced to the body, modifies or impacts the chemical reactions within the body. They may enter the body through many means, including but not limited to:
While you may think of drugs as exclusively recreational substances, many substances fit in this category, including caffeine, alcohol and many medicines used daily.
Medicines are drugs used to diagnose, cure, treat or prevent disease.
The development, manufacture, marketing and use of medicinal drugs is a tightly regulated affair, with the Medicines and Healthcare products Regulatory Agency (MHRA) controlling this in the UK. When people use the term drug discovery and development, they are generally referring to the design and development of new medicines!
Drug discovery is the name given to the process of identifying new potential medications. Traditionally, drug discovery was a somewhat haphazard experience that involved either identifying the active ingredient in traditional medicines or getting lucky.
A drug discovered by identifying the active ingredient in a traditional remedy is the non-steroidal anti-inflammatory drug (NSAID) aspirin. Willow bark and leaves had been used to treat pain and inflammation for thousands of years, with Bayer eventually purifying it and marketing it as a painkiller! Another drug identified from a plant source is the heart medicine digitalis, which is used to help control heart rate and was first isolated from the foxglove plant.
A drug discovered by chance is the antibiotic penicillin. Discovered in 1928 by Alexander Fleming, penicillin was the first widely used antibiotic! Fleming left bacterial plates on the side in his lab when he left for a holiday, returning to find a mould had grown, which killed the bacteria. This was later refined and marketed as the antibiotic penicillin!
Read more about antibiotics and their importance in our article Uses of Antibiotics.
Modern drug discovery is a much more controlled process, using rapid screening processes to rapidly assess several compounds for biological activity. Compounds showing favourable action are then checked for affinity to the desired protein, selectivity to limit side effects, efficacy, metabolic stability and bioavailability! Compounds meeting these criteria are then passed into the drug development process.
The field of science covering medicines is called Pharmacology!
This screening process may take the form of classical or reverse pharmacology. Medicines generally focus on impacting a protein involved somewhere in the genesis of a disease! Most of the new drugs we use today are all produced by chemists in labs of pharmaceutical companies, even though the starting points of these drugs may be a natural product extracted from plants, for example.
Classical pharmacology operates a forward process, testing a chemical library of synthesised small molecules or natural products and extracts against cell cultures (in vitro) and whole organisms (in vivo), looking for compounds that exhibit some form of biological effect, known as lead compounds. When one is found, scientists then work to identify the target of the drug.
Reverse pharmacology operates in the opposite direction, taking advantage of recent genetic sequencing and protein production developments that allow potential target proteins for a disease to be identified and produced in large volumes. The previously mentioned compounds are then screened for interactions with the target protein before their biological activity is confirmed through in vitro and in vivo testing. This allows targeting specific diseases and proteins instead of making drug identification a shot in the dark. By understanding the desired target protein/proteins, compounds likely to display interactions can be selected or designed, allowing for increased identification speed.
As our understanding of human health improves, we discover new diseases which require treatment or potential avenues to treat existing diseases. This, along with medicines losing efficacy over time, or new data about side effects, means that a constant stream of new medicines is needed. This means that drug identification and development is a constant process that can be very lucrative whilst also improving patient outcomes.
One key example of medicines losing efficacy over time is antibiotics. Over time, bacteria evolve resistance mechanisms to different antibiotics, which cause the antibiotic to lose its effect against bacteria possessing the resistance mechanism.
For antibiotics to remain effective treatments against these bacteria, new antibiotics must be continually developed! Antibiotic Resistance is one of the most relevant public health challenges we face today and will face in the near future.
Read more about why in the Antibiotic Resistant bacteria article!
Drug development is the process through which a lead compound identified during drug discovery is brought to market as a sellable medication. It is a long and expensive process involving many non-human testing, regulation, and clinical trials.
The drug development process is generally very organised, with each stage having to be completed and showing favourable results before the next step can commence. This helps in multiple ways:
Drug development may be split into two phases. The pre-clinical phase and clinical phase.
The pre-clinical phase of drug development takes a lead compound, which we know exhibits a desirable level of activity against a target molecule involved in a disease, such as a receptor or a bacterial protein, and gathers information on its:
It's this stage that unavoidably uses animal testing. While large amounts of data can be obtained from in vitro testing on cells and tissues, the complex interplay of drug metabolism, absorption, distribution, and toxicity often means that a compound's effects cannot be seen until administered to a living organism.
Pre-clinical testing establishes the chemical and physical properties of the compound, allowing for the scaling up of manufacture from lab amounts to those sufficient to market the product. These tests also help researchers determine the best way to deliver the medication to patients.
Pre-clinical testing also assesses the toxicity of the new chemical entity (NCE) to major organs and any other areas of the body that are likely to be affected by the drug. If the lead compound is to be taken to clinical trials, it also informs the initial dose and schedule to be administered to the first human, known as the first human dose.
The clinical phase of drug development is the first time the new drug will be administered to a human. This phase is sub-divided into different phases, each with different numbers of participants with different levels of health and varying doses.
At this stage, the new drug is known as an IMP or Investigational Medical Product. Drug development may be broken off at any stage of the trial process as further information about the drug's activity comes to light.
Phase 1 trials are usually non-random trials, with the drug being administered to a cohort of approximately 20 to 80 healthy volunteers to evaluate the safety and dosing of the drug. This is done through a dose-escalation study, where patients are given a very low dose gradually stepped up across participants to calculate the ideal dose. This means participants 1-5 may receive 100 mg, 6-10 150 mg, 10-15 200 mg, and so on. As the doses are stepped up, side effects are monitored to prevent excessive side effects from occurring in high doses.
If the expected side effects are expected to be so severe that giving even a low dose to healthy people is not possible, patients with the targeted condition may be used. An example is testing new chemotherapy drugs where no one without cancer would be used due to the drug's side effects.
This stage may be pre-empted by a smaller trial, known as a phase 0 trial, which aims to evaluate a specific aspect of the drug in humans by giving very few participants a very low drug dose.
Phase two clinical trials utilise a cohort of a few hundred people suffering from the condition the IMP targets. This stage further refines the dosage data and evaluates the IMP's effectiveness in treating the desired disease. If the disease being targeted possesses multiple variants, such as cancer, participants with multiple variants of the disease may be recruited.
Phase three clinical trials further expand the number of participants to a few thousand, all with the targeted disease. This may involve patients across multiple cities or even countries. Phase three continues to identify the best targeted variants with an IMP and gives more info on how the treatment impacts those taking it and what side effects they may have.
This is the last phase of testing before an IMP is released to the market for use in treating patients. If the results of the clinical trials are favourable, the regulatory body will allow the manufacturer to release the medicine. They may place restrictions on the availability or use of the medication, however, depending on the information gained from the trials.
While phase 3 trials are the last trials before a drug is brought to market, the process does not end there. The marketing of a drug exposes many people from a more diverse set of backgrounds than those who may have been selected for earlier trials. This increased sample size means that the effects of the medicine must be observed after its release in a process known as post-market surveillance. It forms part of the pharmacovigilance process and monitors adverse drug reactions.
Pharmacovigilance - The science concerned with the monitoring of adverse effects of medicines. It collects, detects, assesses, monitors and prevents adverse effects from medicines.
Adverse Drug Reactions - A response to a medicine that is unintended, such as unexpected side effects or the severity thereof, or if the drug is less effective at treating a condition than expected when given at the correct dose.
Post-market surveillance is crucial to ensure the continued safety of a medicine. It helps to confirm the efficacy and safety of a medicine whilst gathering data on interactions with other medicines or conditions. From data collected during this stage, the use of a drug may be changed or limited. It may result in changes to dosages used, conditions treated, or who can be given the medicine. It may also reveal that the drug can be used to treat other conditions for which it has not previously been used.
Bias mustn't impact the outcome of a clinical trial as it is crucial for safety. A company that has spent millions of pounds developing a drug is likely to want to get it to market, and so, even if they don't intend to, may introduce bias to the clinical trials. Randomisation and blinding help mitigate the effects of bias in the drug development process.
Patients are randomly and blindly sorted into different groups, with some receiving the new drug, and others receiving a placebo or the current gold standard treatment. This allows researchers to remove bias and gauge the drug's efficacy compared to current treatments or the placebo effect.
Randomisation - The random assignment of participants to different groups to prevent bias towards one group.
Placebo - A placebo is an inert substance given to patients assigned to the group who are not receiving the new drug. This ensures that the patient and possibly the researchers are unaware of which participants receive the actual drug whilst also examining the impact of the placebo effect.
Placebo Effect - Phenomenon by which patients that believe they are receiving a treatment, even if it is inert and so has no medicinal effect, experience some improvement in their symptoms.
Blinding - one or more parties involved in a trial are unaware of what group a patient is in to prevent the influence of results. There are several variants of blinding, covered in the table below.
Level of Blinding: | Who is Blinded |
Single-Blind | Participants are unaware of what group they are in. |
Double-Blind | Participants and those gathering the data are unaware of what group participants are in. |
Triple-Blind | Participants, data collectors and data analysts are unaware of what group participants are in. |
Quadruple-Blind | Participants, data collectors, data analysts and outcome assessors are unaware of what group participants are in. |
The drug discovery and development process is quite straightforward yet also complicated, so we have outlined the process in the below flowchart to provide an ideal, easy-to-follow overview of the process from start to finish.
Drug discovery is the process of finding new drugs whilst drug development tests them through 3 stages of preclinical and clinical trials to ensure that they can be used safely and effectively in humans.
Drug development is essential as it helps us to combat new illnesses, and to find medications that are more effective with less side effects.
Drug development is split into the pre-clinical and clinical phase. The latter is further divided into phases one to four, with each exposing larger and larger pools of people to the drug.
Flashcards in Drug development44
Start learningWhat is Radioimmunotherapy?
mAbs carry radioactive drugs/particles to target antigen cancer cells.
mAbs can be used to locate a specific molecule in a cell/tissue. True or False?
True
What does humanizing mAbs mean?
Engineering mAbs to be more similar to human Monoclonal antibodies.
How do scientists detect the presence of a specific target molecule after binding with a mab?
Fluorescence
Why is humanizing mAbs important?
It lessens the probability of the external antibodies being rejected and attacked by the immune system.
mAbs have been particularly effective therapeutics in modulating the activity of what system:
Immune system

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in