
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Venture into the intricacies of the Ebola Virus with this comprehensive study. You'll start by understanding what the Ebola Virus is, delve into its complex structure, and decode its genetic makeup. Following this, explore how the virus spreads, the symptoms to look out for, and diagnostic methods used for detection. The subsequent sections will equip you with the latest in Ebola Virus treatment options and the importance of preventive measures. Finally, draw crucial lessons from past outbreaks through real-life case studies.
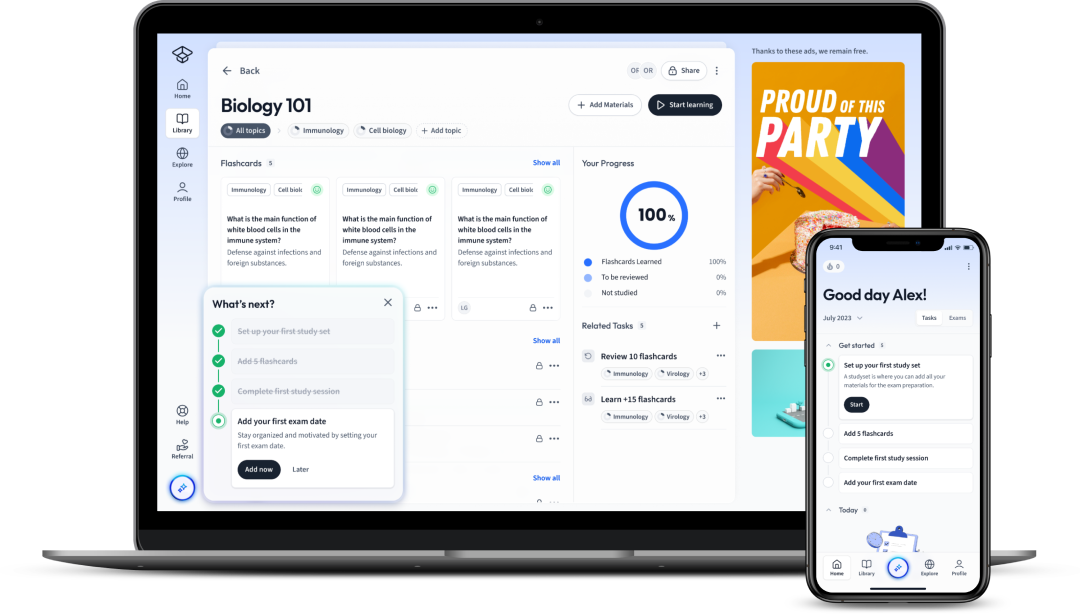
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenVenture into the intricacies of the Ebola Virus with this comprehensive study. You'll start by understanding what the Ebola Virus is, delve into its complex structure, and decode its genetic makeup. Following this, explore how the virus spreads, the symptoms to look out for, and diagnostic methods used for detection. The subsequent sections will equip you with the latest in Ebola Virus treatment options and the importance of preventive measures. Finally, draw crucial lessons from past outbreaks through real-life case studies.
In the realm of microbiology, the Ebola virus represents a fascinating yet enigmatic viral entity. This virus often captures the imagination of many due to its lethal nature and propensity for causing devastating outbreaks, such as the West African epidemic from 2014-2016.
The Ebola virus is a pathogen belonging to the Filoviridae family. This group of viruses is known for causing severe hemorrhagic fever in humans and other primates. Discovered in 1976 near the Ebola River in what is now the Democratic Republic of Congo, this virus poses a severe public health threat.
Strikingly, there are currently five recognised species of the Ebola virus:
The species differ in their geographical distribution, hosts, and severity of disease in humans. The Reston ebolavirus, for example, is the only species known to not cause disease in humans.
A complete comprehension of the Ebola virus structure can provide invaluable insights into its ability to infect host cells and subsequently cause disease.
The Ebola virus is an RNA virus, meaning its genetic material is composed of ribonucleic acid rather than deoxyribonucleic acid (DNA). The virus has a single-stranded, negative-sense RNA genome. This genome holds the code for seven structural proteins which are crucial for the virus' lifecycle.
This implies that its RNA is an inverse copy of the usual mRNA (messenger RNA) that would be used by cells to synthesis virus proteins, which can be represented by the equation: \[ \text{{viral RNA}} + \text{{host machinery}} \rightarrow \text{{viral proteins}} \]
The genome size of the Ebola Virus measures approximately 19,000 base pairs, encoding for seven genes in the following order: NP (nucleoprotein), VP35 (polymerase cofactor), VP40 (matrix protein), GP (glycoprotein), VP30 (transcription activator), VP24 (secondary matrix protein), and L (RNA-dependent RNA polymerase).
The physical form of the Ebola virus is as intriguing as its genetic constitution. From a morphological standpoint, the virus particles (virions) are often long and filamentous, with a characteristic U-shape or '6' shape. This striking morphology is unique to filoviruses, setting them apart from most other virological families.
The virus consists of a host-derived lipid bilayer envelope surrounding a nucleocapsid complex (the combination of virus RNA and nucleoproteins). The envelope is studded with trimeric glycoprotein spikes that enable the virus to attach and fuse with host cells, beginning the infection process.
| Virus Component | Description |
| Lipid Bilayer Envelope | Provides a protective covering for the virus. |
| Nucleocapsid Complex | Accommodates the virus RNA and nucleoproteins. |
| Glycoprotein Spikes | Enable the virus to attach and fuse with host cells. |
The Ebola virus has an intricate and complex structure, with each of its components playing critical roles in its infectivity and pathogenicity. This complexity is what makes it a formidable pathogen, but also presents potential targets for therapeutic intervention.
The eco-epidemiology of Ebola Virus Disease (EVD) explores how environmental factors and interactions between species contribute to the occurrence and spread of the disease. Comprehending these aspects is critical for the prediction, prevention, and control of EVD outbreaks.
Although the precise natural reservoir of the Ebola virus remains unknown, scientific consensus suggests that fruit bats, particularly species belonging to the genera Hypsignathus monstrosus, Epomops franqueti and Myonycteris torquata, may play a crucial role in maintaining the virus in nature. These bats can shed the virus in their saliva and faeces, subsequently infecting other animals or humans that come into contact with these materials.
Regarding the inter-species transmission, the virus can pass to humans following close contact with the blood, secretions, organs, or other bodily fluids of infected animals. The animal species typically involved in this inter-species transmission chain are non-human primates (such as monkeys and chimpanzees) and duikers, which proved to be infected by consumption of 'bushmeat'.
It is also noteworthy that the spread of the virus among human populations is usually initiated by a single introduction of the virus from an animal source.
Index Case: The first human infected in an outbreak.Ebola virus transmission then occurs from person to person through direct contact with the blood, secretions, organs, or other bodily fluids of infected individuals.
Interactions between humans and wild fauna, particularly in the context of hunting, butchering, and consumption of 'bushmeat', logistic an important pathway for the initial spillover of the Ebola virus from animal hosts to humans. In some African communities, hunting and consuming wild animals, including non-human primates and bats, are longstanding practices that can expose humans to the virus.
Human activities such as forest encroachment and habitat destruction might also increase the interface between humans and potential reservoir species, thus elevating the risk of virus spillover events. In the case of fruit bats, for example, the loss of their natural habitats may force them closer to human habitations and agricultural fields, potentially leading to an increased incidence of EVD.
Following the initial transmission of the Ebola virus from an animal to a human (the index case), the virus can spread to other humans via person-to-person transmission. This is primarily driven by close and unprotected contact with the bodily fluids of an infected person.
Transmissions can occur when these fluids, carrying the virus, come into direct contact with the mucous membranes or broken skin of a non-infected person. This can happen through caring for an ill person, sharing personal items, eating from the same plate, or participating in traditional burial rites of a person who has died from EVD.
Period of Communicability: A period when an infected person can contagious. For Ebola, it extends from the onset of symptoms until the recovery or death of the patient. In survivors, the virus may persist in certain body fluids, such as semen and breast milk, for weeks to months following recovery.
Healthcare settings can also facilitate human-to-human transmission when standard precautions, including hand hygiene and use of personal protective equipment, are not strictly practised. Furthermore, unsafe injection practices and lack of sterilisation of medical equipment also contribute to the spread in such contexts.
Adherence to standard protocols for handling patients with suspected Ebola cases and the strict use of personal protective equipment can drastically reduce the risk of transmission in healthcare settings.
Learning how to detect the Ebola virus in its early stages is essential in mitigating its spread and reducing mortality rates. This involves understanding the symptoms of the Ebola virus disease and employing accurate diagnostic tests.
Ebola Virus Disease (EVD), previously known as Ebola Haemorrhagic Fever, presents a range of symptoms best understood in terms of their progression. Early recognition of these symptoms can significantly impact the patient’s prognosis and prevention of virus spread.
When a person becomes infected with the Ebola virus, they pass through what is known as the incubation period before the onset of symptoms. This period can range from 2 to 21 days (with an average of 8 to 10 days), and during this time, the person is not infectious. The incubation period is followed by the emergence of non-specific symptoms.
These initial symptoms are often indistinguishable from other common illnesses, making early diagnosis challenging. As the disease progresses, individuals may experience:
External Bleeding: This is the most distinctive symptom of Ebola and is characterised by bleeding from the eyes, ears, nose, or mouth. Bleeding also can occur from injection sites or rashes. Internal Bleeding: This symptom manifests as blood in the vomit or faeces of the patient, and it can be severe enough to cause organ failure and death.
Detecting Ebola virus requires precise diagnostic tests because the early symptoms of EVD are often non-specific and can resemble other diseases endemic in Ebola-affected areas, such as malaria and typhoid fever. This section comprises laboratory diagnostic methods and the challenges associated with early detection.
When Ebola is suspected based on the symptoms and travel or exposure history, laboratory testing is needed to confirm the diagnosis. In the early stages of infection (about three to ten days after the first symptoms onset), diagnosis is usually made using the following methods:
RT-PCR: Reverse transcriptase polymerase chain reaction is a laboratory method widely used in diagnostics and research for detecting and quantifying specific genetic material in an individual's blood, tissue, or other body fluids.
Ebola diagnosis poses several challenges. Owing to the wide range of symptoms that can mimic other infectious diseases, clinical diagnosis without laboratory confirmation can lead to misdiagnosis.
Moreover, the sensitivity of diagnostic tests varies with the stage of the disease and the presence of symptoms. For instance, RT-PCR is not useful during the incubation period, as viral load in the bloodstream is too low to detect. This can result in false negatives if tested too early after exposure.
Another significant challenge is the requirement for a high-level biosafety laboratory to perform virus isolation and certain other tests, which might not be readily available in regions where EVD outbreaks usually occur.
In addition to these, interpretation of laboratory results should be done judiciously. For example, the presence of antibodies in the patient's blood could indicate either a past or current infection. Similarly, detection of viral RNA or antigens shows only that the virus is present, but it doesn't prove that the virus is causing the symptoms observed.
Addressing these diagnostic challenges needs globally coordinated effort, which includes refinement of diagnostic methods, building local capacity for testing, and strengthening healthcare infrastructure in high-risk regions.
In the fight against the Ebola Virus Disease (EVD), various treatment options have been explored, ranging from the medicinal to support measures. Discovering efficacious treatments has been essential to curb the high fatality rates associated with EVD and to manage outbreaks more effectively.
Due to the versatile nature of the Ebola virus and the severity of the disease it causes, crafting an effective treatment strategy involves an extensive approach. This generally includes medical interventions such as vaccines and antiviral drugs, as well as supportive care measures to manage clinical complications associated with EVD.
About vaccine development, rVSV-ZEBOV-GP \(rVSV\deltaG-ZEBOV-GP\) and Ad26.ZEBOV/MVA-BN-Filo have shown promise. The former is a recombinant, replication-competent Ebola vaccine, while the latter employs a heterologous prime-boost regimen to stir an immune response.
It's worth noting the rVSV-ZEBOV-GP vaccine, also known as Ervebo, is the first Ebola vaccine to get approval from the U.S Food and Drug Administration (FDA) and the European Medicines Agency (EMA). It has reported an efficacy rate of 97.5% and vastly used in the Democratic Republic of Congo (DRC) and Guinea in addressing EVD outbreaks.
In addition to vaccines, antiviral drugs also play a vital role in the therapeutic arsenal against EVD. These are specifically designed to disable the ability of the virus to replicate within human cells. Here are a few noteworthy ones:
Out of these, an important development is the REGN-EB3, which showed superior results in a clinical trial conducted during the 2018-2020 Ebola outbreak in the DRC. Subsequent analysis revealed higher survival rates among patients who received REGN-EB3 or mAb114 compared to those administered with Remdesivir or ZMapp.
Supportive care is a vital pillar in EVD treatment regimen, critical not only to manage the severe symptoms but also to improve overall survival rates. Patients with EVD often suffer from dehydration due to vomiting and diarrhoea, making immediate replenishment of fluids and electrolytes crucial.
Oral rehydration salts or, in severe cases, intravenous (IV) fluids are often used to fulfil this requirement. Maintaining oxygen status and blood pressure, treatment of any concomitant infections, and providing balanced nutrition also forms part of essential supportive care.
Paying attention to a patient's mental health is crucial too, as EVD sufferers may experience psychological distress and could benefit from counselling.
Effective patient isolation and stringent adherence to infection prevention and control measures are critical not only to provide a safe environment for the patients but also to prevent transmission of the virus to healthcare staff and others.
Achieving breakthroughs in EVD treatment regimens has been the result of relentless research efforts. However, there is still substantial room for the development of more effective treatment strategies.
Research is still underway to find drugs that can target various stages in the Ebola virus life cycle. Exploring an assortment of therapeutic options, such as antiviral drugs, immune therapy, and biologic therapy has the potential to provide new avenues for EVD treatment.
Improving the potency and breadth of vaccines also holds key importance. Work is being done on designing vaccines that can provide lasting immunity and guard against multiple species of the Ebola virus.
Unravelling the pathogenesis of the Ebola virus at the molecular level can contribute to the understanding of how the virus affects the human body and identify potential targets for therapeutic intervention. Research in this area, combined with collective long-term surveillance and continued investment in the healthcare infrastructure of at-risk regions, will be pivotal for the comprehensive mitigation of EVD in the future.
In an effort to curtail the Ebola Virus Disease (EVD), various preventive measures have been implemented worldwide. These range from practices in healthcare centres to increased public awareness and maintaining high hygiene standards.
Given the virulence of the Ebola virus and its high transmission rate, the establishment of robust containment methods and comprehensive guidelines is imperative for preventing EVD outbreaks.
Healthcare centres form the frontline in the battle against EVD, and upholding stringent biosafety and infection control measures in these settings is pivotal to prevent nosocomial transmission of Ebola and protect healthcare workers.
Firstly, healthcare personnel must use personal protective equipment (PPE) appropriately. This typically includes gloves, masks, gowns, and eye protection. The World Health Organisation (WHO) eventually recommends double gloving, waterproof aprons, and respiratory protection in certain high-risk situations.
Secondly, it's essential to apply standard safety precautions in health facilities to prevent Ebola transmission. This involves:
Apart from these, incorporation of stringent infection control policies, including sterilisation practices, management of healthcare waste, and handling of deceased patients, is of paramount importance.
Social mobilisation and heightening public awareness plays a critical role in preventive efforts against Ebola transmission. A significant part of EVD prevention involves educating the general public about the nature of the disease, its transmission routes, and preventive actions individuals can take.
Simple actions such as personal hygiene, avoiding direct contact with EVD patients or their body fluids, not touching objects potentially contaminated by an infected person's body fluids, avoiding contact with bodies of deceased EVD patients, and informing healthcare professionals immediately when symptoms are present can significantly mitigate the risk of Ebola transmission.
Furthermore, increasing public awareness about the importance of reporting suspected cases immediately to the health authorities is crucial to facilitate early detection, reliable contact tracing, and prompt isolation and treatment of the cases.
Hygiene promotion is another significant aspect of EVD prevention. Implementation of community-led sanitation programmes, safe management of water supplies, and improved hand-washing facilities at community and institutional levels are instrumental in curbing the disease transmission.
Past outbreaks of EVD have provided invaluable learnings and insights on disease control. By studying these outbreaks, one can understand better the effectiveness of preventive strategies, challenges encountered, and lessons learned - knowledge that is crucial for formulating future preventive measures.
Recognition of community-based case management operations and initiation of 'safe and dignified burials' emerged as significant breakthroughs from the 2014-2016 West Africa Ebola outbreak. The success of the ring vaccination strategy during the 2018-2020 DRC Ebola outbreak underscores the role of vaccines in preventing EVD.
An important aspect of case studies involves understanding the role risk communication played in these outbreaks. This ensures the delivery of accurate, timely and credible information to the public and fosters trust between communities and public health responders.
Crucially, these case studies illuminate the need for long-term investment in healthcare infrastructure and human resources at the global and local levels, which are vital for strengthening disease surveillance and maintaining high levels of preparedness to respond to future outbreaks.
Flashcards in Ebola Virus15
Start learningWhat family does the Ebola virus belong to and what is it known for causing?
The Ebola virus belongs to the Filoviridae family and is known for causing severe hemorrhagic fever in humans and other primates.
What is the nature of the Ebola virus genetic material?
The Ebola virus is an RNA virus with a single-stranded, negative-sense RNA genome, which holds the code for seven structural proteins.
What is the physical structure of the Ebola virus?
The Ebola virus has a host-derived lipid bilayer envelope, a nucleocapsid complex housing the virus RNA and nucleoproteins, and glycoprotein spikes that enable the virus to attach and fuse with host cells.
What do we know about the origins and transmission of the Ebola Virus?
The natural reservoir of the Ebola virus is thought to be fruit bats, which can shed the virus in their saliva and faeces. Interestedly, the spread of the virus among humans is usually initiated by a single introduction of the virus from an animal source.
What is the role of animals, and their interactions with humans, in the spread of the Ebola virus?
Interactions between humans and wild fauna, particularly regarding the hunting, butchering, and consumption of 'bushmeat', can expose humans to the Ebola virus. Forest encroachment and habitat destruction can also increase this interface, potentially leading to more frequent virus spillover events.
How does human-to-human spread of the Ebola virus occur?
After the initial transmission from an animal, the Ebola virus can spread to other humans through close and unprotected contact with the bodily fluids of an infected person. This can occur in various settings, including healthcare setups, familial caregiving, or traditional burial rites.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in