
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Delve into the fascinating world of microbiology with a comprehensive exploration of hepatitis viruses. Gain a deeper understanding of the hepatitis A, B, and C viruses, exploring their unique structures, classifications, transmission methods, and effects on global health. Educate yourself on the structural components of these viruses, and understand how they are classified according to different factors. Additionally, learn about the impact of these viruses on communicable diseases worldwide and dig into strategies employed to counteract transmission. The knowledge base you're about to build will pave your way to comprehending one of the most impactful issues in the realm of infectious diseases.
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDelve into the fascinating world of microbiology with a comprehensive exploration of hepatitis viruses. Gain a deeper understanding of the hepatitis A, B, and C viruses, exploring their unique structures, classifications, transmission methods, and effects on global health. Educate yourself on the structural components of these viruses, and understand how they are classified according to different factors. Additionally, learn about the impact of these viruses on communicable diseases worldwide and dig into strategies employed to counteract transmission. The knowledge base you're about to build will pave your way to comprehending one of the most impactful issues in the realm of infectious diseases.
Hepatitis Viruses are a group of diseases known to attack the liver causing inflammation. In this guide, you will learn about the primary strains, namely Hepatitis A, B, and C.
You may already understand that Hepatitis A, B and C are viral diseases, but in order to gain a more comprehensive understanding, it's important to take a closer look at each one.
Hepatitis A is predominantly spread via food or water that's been contaminated by faecal matter from an infected person.
On the other hand, Hepatitis B is usually transmitted through contact with infected bodily fluids like blood or semen. It could potentially be a long-term, chronic infection leading to severe illness such as cancer or cirrhosis of the liver.
Lastly, Hepatitis C is commonly spread through direct contact with the blood of an infected person. It is usually a long-term disease and can lead to liver damage or even liver cancer.
While this overview provides a basic understanding of Hepatitis A, B, and C, let's delve deeper into their key differences and similarities.
The available vaccines against Hepatitis A and B have significantly reduced the occurrence and severity of these diseases. Unfortunately, as of now, there is no established vaccine for Hepatitis C.
The Hepatitis A, B, and C viruses while all affecting the liver, vary in their mode of transmission, severity, treatment strategies, and prophylaxis measures, as summarized in the table below:
| Type | Transmission | Severity | Treatment Strategies | Prevention |
| Hepatitis A | Fecal-oral | Mild to Moderate | Symptomatic Relief | Vaccine available |
| Hepatitis B | Infected body fluids | Mild to severe (Chronic infection possible) | Antiviral medication, In severe cases liver transplant | Vaccine available |
| Hepatitis C | Direct contact with infected blood | Mostly severe (Chronic infection common) | Antiviral medication | No vaccine currently available, Avoid sharing needles etc. |
For example, Hepatitis A is usually spread from the consumption of food or water contaminated with the feces of an infected person, while Hepatitis B and C are spread via blood and other bodily fluids.
Though Hepatitis A, B, and C viruses have several fundamental differences, they also share some similarities.
Hepatitis: It is a term that refers to inflammation of the liver. It's commonly caused by a viral infection, but there are other possible causes of hepatitis. These include autoimmune hepatitis and hepatitis that occurs as a secondary result of medications, drugs, toxins, and alcohol.
Their diagnosis also involves similar steps like blood tests to detect specific antigens or antibodies. Recognizing these similarities can help in early detection and appropriate management of these diseases.
The crystal clear understanding of how Hepatitis Viruses are built can aid in their identification, all the while fostering the development of effective therapies and vaccines. Just like any other viruses, Hepatitis A, B and C present unique structural components that contribute to their stability, mode of transmission, and pathogenicity.
Going under the microscope, you can observe detailed attributes of three major Hepatitis viruses involves a comprehensive examination of their structural components. These components, in microscopic terms, are the arrangement of proteins, genetic material, and sometimes a lipid envelope, all contributing to a virus's ability to enter host cells and replicate. This section will detail the structure of Hepatitis A, B and C viruses, highlighting their differences and similarities.
Hepatitis A virus (HAV) is a non-enveloped virus, meaning it does not have a lipid envelope. It is composed by a protein shell known as a capsid, which encloses the virus's genetic material. This intricate structure is rendered using a large number of identical protein subunits, forming a symmetrical icosahedron.
RNA: Ribonucleic Acid. It is a molecule implicated in various biological roles including coding, decoding, regulation, and expression of genes.
The external capsid safeguards the sensitive RNA inside, bestowing the virus with further survivability in external conditions. Furthermore, HAV utilises host cellular machinery to replicate its RNA and form new viral particles.
Moving on to Hepatitis B virus (HBV), which is an enveloped virus. It consists of an outer lipid envelope and an inner nucleocapsid, harbouring the viral genetic material.
DNA: Deoxyribonucleic Acid. It is the hereditary material in humans and almost all other organisms. Nearly every cell in a person's body has the same DNA.
The surface envelope contains proteins that enable the virus to bind to and enter host cells. On the other hand, the nucleocapsid inside the envelope contains enzymes necessary for viral replication. Overall, the structure of HBV allows for complex replication mechanisms and the ability to persist in host cells. The outer lipid layer also contributes to the virus's ability to evade the host immune response.
Lastly, Hepatitis C virus (HCV) is also an enveloped virus. It has a similar structure to HBV in terms of having an outer lipid envelope and an inner nucleocapsid. However, the key difference lies in their genetic material.
Its envelope, which encloses the nucleocapsid, carries proteins known as glycoproteins.
Glycoproteins: These are proteins that have sugar molecules (oligosaccharides) attached to them. They play essential roles in cell-to-cell recognition in the immune response and in the body's reaction to disease.
Just as biologists classify organisms into distinct groups based on their characteristics, virologists also classify viruses to help us understand them better. This classification often includes the type of nucleic acid, structural characteristics, mode of replication, host organisms, and the type of diseases they cause. When it comes to Hepatitis viruses, the classification becomes particularly nuanced considering the significant differences between Hepatitis A, B and C viruses.
Starting with the genus to which all hepatitis viruses belong, namely Hepatovirus for Hepatitis A and Orthohepadnavirus and Hepacivirus for Hepatitis B and C respectively. However, the distinction doesn't end there, we can further characterise them based on their nucleic acid types, genome structure, replication mechanisms, and presence of envelope.
Classification of viruses including the Hepatitis A, B, and C viruses, involves incorporating various virological and clinical factors, including the nature of their genomic material, capsid symmetry, envelope presence, replication cycle, and pathogenesis in the host.
A capsid is the protein shell of a virus. It consists of several oligomeric structural subunits made of protein called protomers. The observable 3D morphological or symmetry unit is termed as the capsomere.
Typically, Hepatitis A is classified by its RNA genome and non-enveloped characteristics. Whereas, Hepatitis B is defined by a partially double-stranded DNA genome and its enveloped nature. Hepatitis C, on the other hand, is covered by a lipid envelope and contains a positive-sense RNA genome.
The methodology also extends to serological tests. Since atypical immune response is characteristic of many viral infections, detecting specific antibody presents in the infected host formed against the viral antigens aids in identifying the type of viral strain.
Several determining factors contribute to the classification of Hepatitis viruses. Here we elaborate on a few critical ones:
Interestingly, the evolution of genomic sequences is a powerful tool in classifying and tracking viral origins.
When it comes to hepatitis viruses, understanding the transmission methods is of paramount importance. Since Hepatitis A, B, and C viruses each have a unique mode of transmission, gaining insights into how these viruses spread can play a crucial role in formulating preventive strategies and raising awareness.
Hepatitis A virus (HAV) primarily disseminates through the faecal-oral route. The term 'faecal-oral' indicates that the virus, shed in the faeces of an infected individual, is ingested by another person. This can happen through several situations:
Hepatitis A is a hearty virus, capable of surviving for extended periods outside the human body. It can also resist freezing and withstand temperatures up to 60°C, highlighting the importance of adequate heating during cooking to kill the virus. Hepatitis A outbreaks commonly occur in overcrowded settings or regions with poor sanitation facilities.
The primary transmission channels of Hepatitis B Virus (HBV) are quite different from those of HAV. HBV is a blood-borne virus, highly infectious, and can be transmitted in several ways:
| Perinatal Transmission | Commonly referred to as "mother-to-child" transmission, this occurs when an infected mother passes the virus to her baby during delivery. |
| Blood and Body Fluids Exposure | This can occur through a needlestick injury in healthcare settings, sharing needles, syringes, or drug-injection equipment, or through exposure to the blood or open sores of an infected person. |
| Sexual Transmission | HBV can be spread through sexual contact with an infected person without using a condom. The virus can also be transmitted from men to women and among men who have sex with men. It is 50-100 times more infectious than HIV. |
It's significant to note that casual contact, such as sharing eating utensils or hugging, does not spread HBV. Unlike HAV, this virus needs a direct route of entry into the blood to cause infection.
Similar to Hepatitis B, Hepatitis C Virus (HCV) is also a blood-borne virus, primarily transmitted through direct contact with the blood of an infected person. The following are the primary pathways for the transmission of HCV:
Notably, HCV is not spread through breast milk, food, water, or casual contact. The virus is quite robust, capable of surviving outside the body at room temperature, on environmental surfaces, up to several weeks.
To further understand the biology of Hepatitis viruses and their impact on global health, one needs to delve into topics such as viral evolution and mutation and the broader global implications on communicable diseases. The following sections will unravel these subjects.
Understanding the principles of viral evolution and mutation is pivotal to grasp the epidemiology, pathogenesis and, ultimately, the control of Hepatitis viruses. Just as species evolve to adapt to their environments, viruses, including Hepatitis viruses, undergo evolution to survive and proliferate. The high mutation rates in viruses result from their rapid replication and the lack of proofreading mechanisms during replication.
Viral mutations refer to any changes in the genetic sequence of a virus. These changes can occur naturally during reproduction, and when advantageous, they become more prevalent in the viral population. The three Hepatitis viruses significantly differ in their mutation rates due to their distinct replication mechanisms and genetic material, affecting their infectivity and virulence. Let's understand the mutation and its impact in detail:
These mutation-driven changes in Hepatitis viruses can significantly affect disease severity, transmission and response to therapies, making detailed understanding paramount for effective disease control.
As RNA and DNA viruses, HAV, HBV and HCV have distinct evolutionary patterns. The evolutionary patterns offer insights into the origin and genetic diversity of the viruses, and can even aid in designing control strategies and therapeutic interventions.
| Hepatitis A Virus: | HAV is classified into six genotypes, with three infecting humans. Despite its high mutation rate, strong purifying selection preserves its overall genetic stability. The geographical distribution of different genotypic variants helps track the origin of outbreaks. |
| Hepatitis B Virus: | HBV evolution is driven by mutation and natural selection, leading to ten diverse genotypes. Certain genotypes are associated with a higher risk of liver disease, while others are linked to specific geographical areas, aiding in tracking the virus's spread. |
| Hepatitis C Virus: | HCV's evolution is characterised by the generation of a diverse range of quasispecies. Genotypic and sub-genotypic variations in HCV are associated with differences in disease progression, responsiveness to antiviral therapy, and geographic distribution. |
The understanding of these evolutionary patterns can shed light on the forces shaping the viral genetic diversity and contribute to effective disease management.
Hepatitis viruses pose substantial public health challenges, leading to significant morbidity and mortality worldwide. Understanding the global implications aids in conceptualising strategies to manage the spread of these infectious diseases.
The prevalence and impact of hepatitis viruses vary globally, with certain populations and regions bearing a higher burden than others. To put it in perspective:
A comprehensive understanding of these global statistics can aid in framing targeted regional strategies to curb the spread of these infectious diseases.
Given the magnitude of hepatitis virus-related diseases, effective strategies for prevention and control are critical. Some effective strategies include:
These strategies underscored the importance of a multifaceted approach to control the transmission of Hepatitis viruses globally.
Flashcards in Hepatitis Viruses15
Start learningWhat are Hepatitis A, B and C viruses and how are they transmitted?
Hepatitis A, B and C are viral diseases that attack the liver. Hepatitis A is spread via contaminated food or water, Hepatitis B through contact with infected bodily fluids like blood or semen, and Hepatitis C through direct contact with infected blood.
What are some key differences between Hepatitis A, B, and C?
These viruses vary in their mode of transmission, severity, treatment strategies, and prophylaxis measures. Hepatitis A is generally mild, and a vaccine is available. Hepatitis B can be severe, is treated with antiviral medication, and a vaccine is available. Hepatitis C is usually severe, is also treated with antiviral medication, but no vaccine is currently available.
What are some similarities among Hepatitis A, B and C viruses?
All three types of Hepatitis cause inflammation or swelling in the liver and often present similar initial symptoms like fatigue, loss of appetite and fever. They are also diagnosed using similar steps such as blood tests to detect specific antigens or antibodies.
What are the structural components of Hepatitis A Virus (HAV)?
The Hepatitis A Virus (HAV) is non-enveloped and contains a protein shell, known as a capsid, which encloses the virus's genetic material, single-stranded RNA. This structure gives the virus the ability to survive in external conditions.
What distinguishes the structure of the Hepatitis B Virus (HBV) from other hepatitis viruses?
The Hepatitis B Virus (HBV) is an enveloped virus, containing an outer lipid envelope, an inner nucleocapsid, and a partially double-stranded DNA genome. The structure allows for complex replication mechanisms and the ability to persist in host cells.
How does the structure of the Hepatitis C Virus (HCV) facilitate its infection?
Hepatitis C virus (HCV) is an enveloped virus with a single-stranded RNA genome. Its envelope carries glycoproteins that helps it enter host cells. Unlike HBV and HAV, HCV can integrate its genetic material into the host cell's genome, leading to chronic infection.
Already have an account? Log in
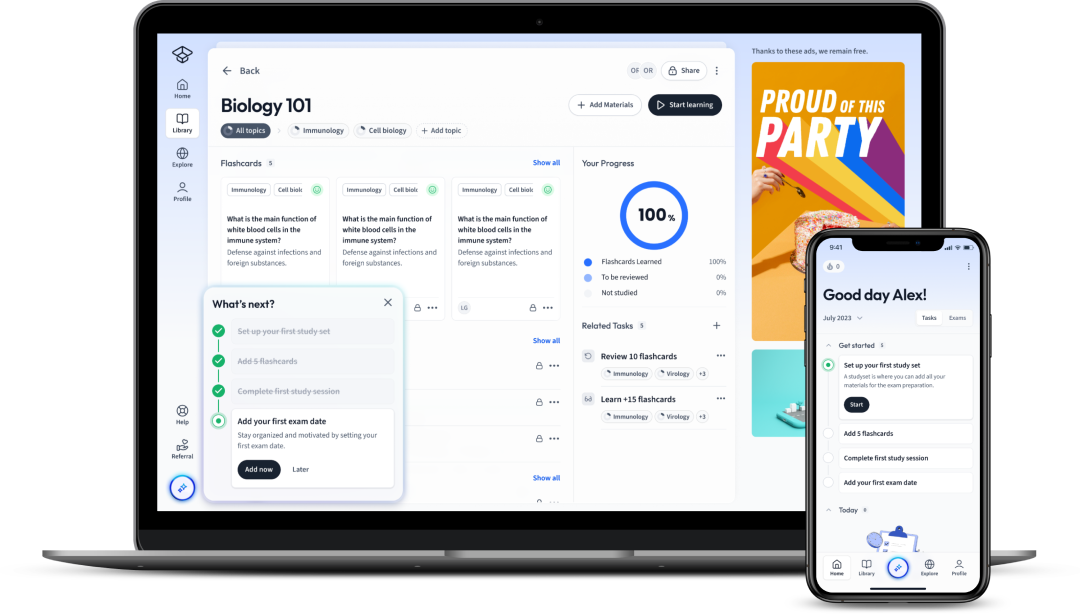
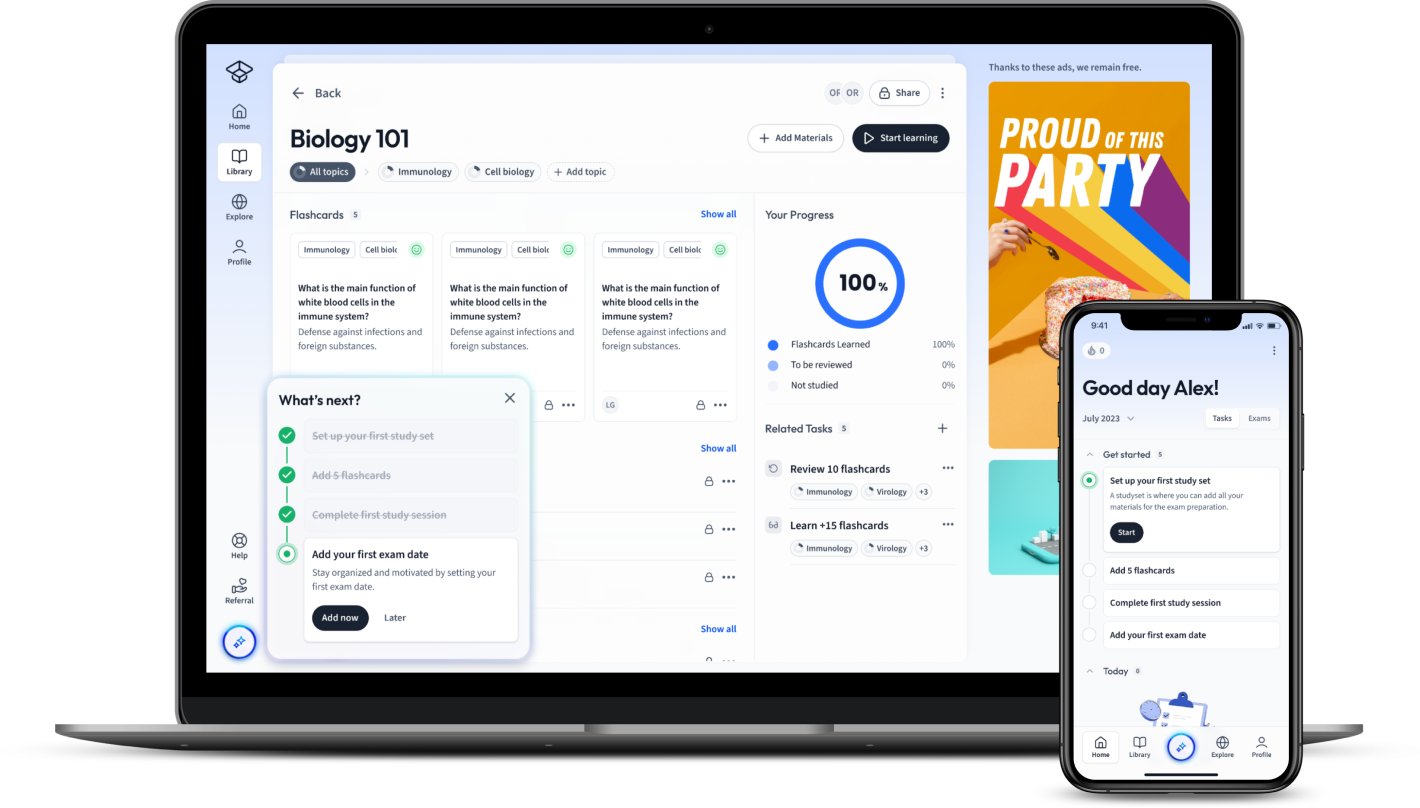
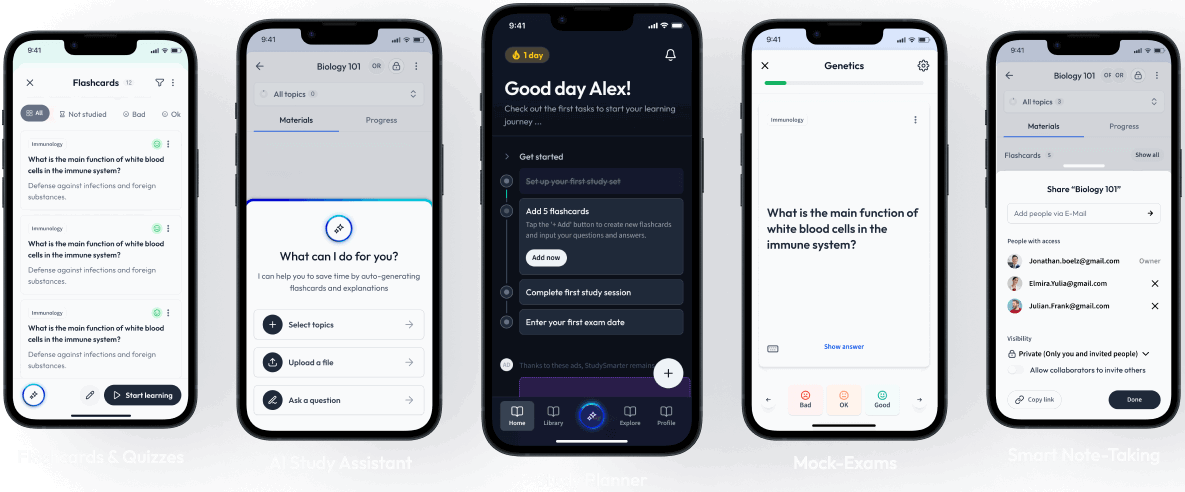
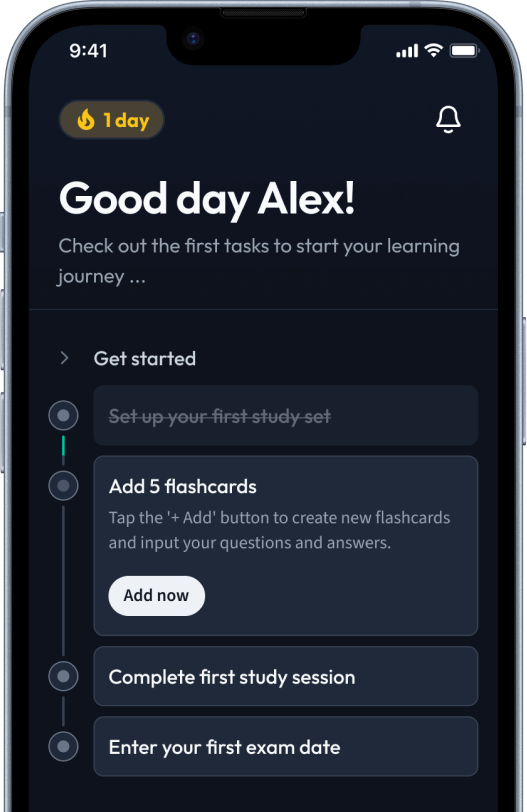
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in