
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Dive into the fascinating world of Intracellular Bacteria - miniature life forms that thrive within the cells of larger organisms. This detailed piece will provide you with comprehensive knowledge about their classifications, operating mechanisms, and the diseases they can cause. You'll also discover the role of antibiotics in treating infections caused by these intriguing microorganisms. Empower your understanding and confront the microbial world head-on through this deep exploration of Intracellular Bacteria.
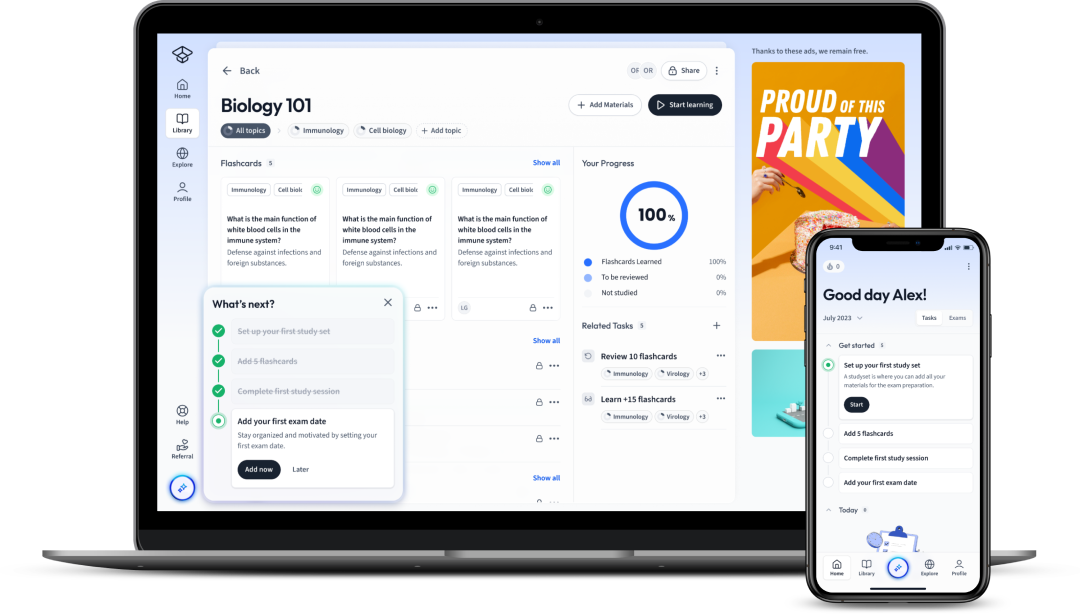
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDive into the fascinating world of Intracellular Bacteria - miniature life forms that thrive within the cells of larger organisms. This detailed piece will provide you with comprehensive knowledge about their classifications, operating mechanisms, and the diseases they can cause. You'll also discover the role of antibiotics in treating infections caused by these intriguing microorganisms. Empower your understanding and confront the microbial world head-on through this deep exploration of Intracellular Bacteria.
When you embark on the journey to understand the biology of bacteria, an interesting concept often encountered is that of 'Intracellular Bacteria'. As you may have guessed, these are bacteria that reside within other cells. This fascinating category of bacteria has developed unique mechanisms to invade and survive within host cells, which can make them particularly challenging to treat clinically.
Intracellular bacteria are bacteria that are able to enter, survive and multiply within the cells of a host organism.
Fascinatingly, intracellular bacteria can invade both animal and plant cells, living either in the cytoplasm or within a special vacuole, known as an endosome. Once inside, they can evade the host's immune response and antibiotic treatments. Therefore, understanding these microscopic invaders is vital in the field of microbiology and infectious diseases.
There are two broad categories of intracellular bacteria: Obligate and Facultative. The former are completely dependent on the intracellular environment and cannot live outside host cells. They include bacteria such as Mycobacterium leprae (which causes leprosy) and Chlamydia trachomatis (which causes chlamydia). Facultative intracellular bacteria, on the other hand, can live both inside and outside host cells, making them very adaptable. They include bacteria such as Salmonella enterica and Listeria monocytogenes.
An example of the resilience of these bacteria can be seen in Tuberculosis. Mycobacterium tuberculosis is an obligate intracellular bacteria that resides within lung macrophages, evades the immune response and causes a devastating disease.
Intracellular bacteria can be divided into several categories based on various criteria, including the type of host cell invaded, the localization within the host cell, and the mechanism of invasion and survival. This classification helps scientists devise ways to deal with these bacteria and to understand the diseases they might cause.
Moreover, classifications help determine the bacteria's traits, which are crucial when devising treatments for diseases they cause. For example, some intracellular bacteria use a secretion system called Type III, which injects effector proteins into the host cell to aid in cell invasion and antibody resistance.Did you know? Legionella pneumophila, the bacteria that causes Legionnaires' disease, is a fascinating example of an intracellular pathogen. It invades amoebae in the environment and human macrophages in the lung. To ensure its survival, the bacterium manipulates these host cells to avoid their usual process of killing pathogens.
| Obligate intracellular bacteria | Mycobacterium leprae, Chlamydia trachomatis |
| Facultative intracellular bacteria | Salmonella enterica, Listeria monocytogenes |
| Intracellular mutualists | Wolbachia in insects, Rhizobium in legumes |
As with any living organism, intracellular bacteria have developed sophisticated mechanisms to ensure survival and replication within the host cells. They operate with specific, evolved strategies that let them invade cells, circumvent the host's immune defenses, and finally multiply. This section seeks to elucidate these intriguing mechanisms.
Intracellular bacteria have to cross multiple barriers to successfully infect host cells. They have to first adhere to the cell, then enter it, and finally evade the host’s defenses. Each of these stages requires a different tactical operation.
The first stage of bacterial infection is the adherence of the bacteria to the host cell. This step is critical for infection and is mainly achieved through the formation of specialized structures called pili or fimbriae. These hair-like appendages on the cell surface facilitate the bacteria's binding to the host cell.
In the second stage, the bacteria penetrate the cell membrane using various mechanisms. This includes:After initial entry, bacteria employ strategies to avoid or suppress the host's defenses and survive.
| Method of invasion | Example |
| Phagocytosis | Mycobacterium tuberculosis |
| Trigger mechanism | Salmonella enterica |
The example of Legionella pneumophila can demonstrate the above. This bacteria enters the host cell by tricking it into initiating phagocytosis. However, it then quickly prevents the newly formed phagosome from fusing with the cell's lysosomes - the usual next step in destroying pathogens - ensuring its survival.
Once inside the host cell, intracellular bacteria deploy various survival strategies. They effectively manipulate the host cellular machinery for their advantage.
Some intracellular bacteria can inhibit phagosome-lysosome fusion to avoid destruction by the host's cellular mechanisms. The bacteria thereby remain alive in the phagosome, which is transformed into a bacteria-friendly environment known as a bacterium-containing vacuole (BCV). This BCV provides a protective niche from harmful factors in the cell.
Phagosome-lysosome fusion is the process by which a cell engulfs foreign particles into a phagosome (a small cavity or vesicle), which then fuses with lysosomes, structures in the cell full of enzymes that can break down the captured material. Thus, this mechanism is a major way in which cells deal with and destroy invading bacteria.
Other bacteria, instead of avoiding the lysosome, have evolved to survive its hostile conditions. For instance, the bacteria Coxiella burnetii can resist the harsh, acidic environment within the lysosome, making its way to the cytoplasm where the conditions are more conducive for multiplication.
Also, there is evidence that some intracellular bacteria even regulate cell death to their advantage. They can inhibit the host cell's programmed cell death (apoptosis), promoting their own replication and survival.Embarking on the diverse world of intracellular bacteria, you will come across a wide range of species. Each of these bacterial species exhibits unique mechanisms of intracellular invasion, living, and multiplying. This variability affects their pathogenic potential, disease presentations, and our therapeutic strategies to combat the diseases they cause.
When you talk about intracellular bacteria, some names might immediately spring to you as icons of this group. A few well-known examples are discussed below, including the diseases they cause:
Salmonella enterica: This facultative intracellular bacterium is responsible for salmonellosis, causing symptoms ranging from gastroenteritis to typhoid fever.
Mycobacterium tuberculosis: An obligate intracellular pathogen causing tuberculosis affecting the lungs but can also spread to other parts of the body.
Chlamydia trachomatis: It is an obligate intracellular bacterium causing chlamydia, the most common sexually transmitted bacterial infection worldwide.
Legionella pneumophila: This bacterium is a facultative intracellular organism known for causing Legionnaires' disease, a severe form of pneumonia.
Listeria monocytogenes: A facultative intracellular bacterium, it is linked with listeriosis, a serious infection typically caused by eating bacterium-contaminated food.
The above list is just the tip of the iceberg. Many other intracellular bacteria like Shigella, Rickettsia, Ehrlichia, Coxiella and Brucella, each cause specific diseases and show unique adaptations to intracellular life.
When you go deeper into the world of intracellular bacteria, a significant distinction arises. That's between obligate and facultative intracellular bacteria. Obligate intracellular bacteria are ones that cannot survive outside a host cell. This category includes a variety of bacterial species each widely known for the diseases they cause and their unique survival strategies.
Mycobacterium leprae: This bacterium is the causative agent of leprosy. It is considered an obligate intracellular parasite because it loses its viability rapidly once outside its host cell.
Chlamydia trachomatis: As mentioned earlier, this bacterium causes chlamydia, a sexually transmitted disease. It's an obligate intracellular bacterium because it cannot obtain ATP on its own and relies on the host cell for energy.
Understanding diseases caused by intracellular bacteria is crucial, as these microorganisms are responsible for a wide array of infections that pose significant health challenges worldwide. The illnesses these bacteria cause range from mild and short-lived to severe and chronic, even life-threatening. Considering their potential seriousness and impact on public health, an in-depth exploration of these ailments becomes necessary.
There's a wide range of diseases caused by intracellular bacteria, each with distinct characteristics and clinical manifestations. The distinct nature of these diseases is primarily due to the unique life-cycles, invasion strategies, and survival tactics of the causative bacteria. By delving into a few, you get a snapshot of this intriguing variety.
Tuberculosis: Primarily caused by Mycobacterium tuberculosis, tuberculosis (TB) mainly affects the lungs but can impact other parts of the body. The bacterium survives and replicates in macrophages, evading host immune responses.
Listeriosis: Listeria monocytogenes, a facultative intracellular bacterium, can cause listeriosis. It's often transmitted through contaminated food and can cause severe infections in those with compromised immune systems, the elderly, or pregnant women.
Chlamydia: Caused by Chlamydia trachomatis and Chlamydia pneumoniae, chlamydia infections can result in a range of conditions, from sexually-transmitted infections to pneumonia. The bacteria can manipulate the host cell to create an intracellular niche where they replicate and survive.
Legionnaires' Disease: Legionella pneumophila, a facultative intracellular bacterium, is responsible for this severe form of pneumonia. The bacterium enters and proliferates within alveolar macrophages, leading to lung infection.
Intracellular bacteria play a critical part in communicable diseases, which are conditions that spread from person to person. Several of the diseases caused by these bacteria are infectious, spreading through various modes, including respiratory droplets, sexual contact, or ingestion of contaminated food or water.
For example, tuberculosis is a well-recognised airborne disease. Mycobacterium tuberculosis is transmitted when an infected person coughs, sneezes, or speaks, releasing droplets carrying the bacteria into the air, which can then be inhaled by others in close proximity. Similarly, diseases like chlamydia are sexually transmitted, spreading through intimate contact. The bacterium Chlamydia trachomatis can infect the urethra in men and the cervix in women, causing a range of symptoms. Even foodborne illnesses like listeriosis are communicable diseases, as they originate from eating food contaminated with Listeria monocytogenes. The bacteria can survive and multiply even in refrigerated food, increasing the risk of disease transmission. Moreover, these intracellular bacteria have essential implications for communicable disease control. Their survival tactic of hiding within host cells makes them resistant to many antibiotic treatments as well as the immune system's defences. As such, diseases caused by these bacteria often require long-term treatment and can result in recurring or chronic infections. This characteristic can impact the tracking, treatment, and prevention efforts of these communicable diseases. Understanding these bacteria's mechanisms of infection and survival provides significant insights into disease management strategies, informing antibiotic regimen choices, vaccine development, and preventative strategies like good hygiene practices, safe food handling, sexual health education and screening programs.Antibiotics have been essential tools in our medical arsenal for combating bacterial infections. However, the treatment of infections caused by intracellular bacteria poses unique challenges due to these bacteria’s distinct lifestyle, which allows them to ensconce themselves within host cells. In this section, you will look closely at the antibiotics effective against intracellular bacteria and discuss the challenges faced in treating intracellular bacterial infections.
When dealing with intracellular bacteria, selecting the right antibiotic is a critical aspect of treatment. The antibiotic should not only be toxic to the bacteria but also capable of penetrating host cell membranes to reach the bacterial hideout. The efficacy of several antibiotics against intracellular bacteria varies, and some have been found to be particularly effective.
Tetracyclines: This group of antibiotics, including doxycycline and minocycline, are broad-spectrum bacteriostatic agents. They inhibit bacterial protein synthesis by binding to the 30S ribosomal subunit. Notably, tetracyclines can penetrate cell membranes, making them useful against intracellular bacteria like Chlamydia, Rickettsia, and Mycoplasma. Furthermore, doxycycline is often the drug of choice for treating infections caused by Chlamydia trachomatis, Ureaplasma urealyticum, and Mycoplasma pneumoniae.
Macrolides: Macrolides, such as erythromycin, clarithromycin, and azithromycin, also inhibit bacterial protein synthesis and have a broad spectrum of activity. They are effective against both extracellular and intracellular bacteria, including Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydia trachomatis.
Fluoroquinolones: These synthetic antibiotics, including ciprofloxacin and levofloxacin, interfere with bacterial DNA replication by inhibiting DNA gyrase and topoisomerase IV enzymes. They have excellent penetration ability into host cells and are effective against a range of Gram-positive and Gram-negative bacteria, making them a potent tool against intracellular pathogens such as Legionella, Mycobacterium, and Chlamydia.
Intracellular bacteria have evolved complex mechanisms to evade host immune responses and anti-bacterial drugs, making their treatment particularly challenging. A few prominent obstacles include:
Penetration Barrier: The first challenge is the host cell membrane, which can be a significant barrier to the entry of antibiotics. Only those drugs that can penetrate this membrane to gain intracellular access can effectively tackle these bacteria.
Intracellular Environment: Once inside the host cell, intracellular bacteria usually reside in a modified compartment that shields them from direct contact with antibiotics. For example, Mycobacterium tuberculosis and Salmonella enterica survive within modified phagosomes, which are difficult for antibiotics to penetrate.
Antibiotic Resistance: As with all bacteria, intracellular bacteria also develop resistance to antibiotics, further complicating treatment efforts. Resistance mechanisms include efflux pumps which actively expel antibiotics from the bacterial cell and enzymatic degradation of the antibiotic compound.
Flashcards in Intracellular Bacteria15
Start learningWhat are intracellular bacteria and why are they important?
Intracellular bacteria are bacteria that can enter, survive, and multiply within host cells. They're important because they've developed unique mechanisms to evade the host's immune response and antibiotic treatments, making them hard to treat. Therefore they are a vital area of study in microbiology and infectious diseases.
What are the two broad categories of intracellular bacteria?
The two broad categories of intracellular bacteria are obligate and facultative. Obligate intracellular bacteria are completely dependent on the intracellular environment, while facultative intracellular bacteria can live both inside and outside host cells.
How does the classification of intracellular bacteria help scientists?
Classifying intracellular bacteria based on criteria such as host cell type, localization within the host cell, and invasion mechanism helps scientists understand the diseases these bacteria might cause and devise strategies to deal with them. It also provides insights into bacteria’s traits, vital for treatment development.
What is the first stage of bacterial infection in a host cell?
The first stage of bacterial infection in a host cell is the adherence of the bacteria to the cell, largely achieved through the formation of specialized structures called pili or fimbriae.
What is phagosome-lysosome fusion, and how do certain bacteria respond to it?
Phagosome-lysosome fusion is a cellular process where a cell engulfs foreign particles into a phagosome, which then combines with lysosomes, full of enzymes that break down the captured material. Some intracellular bacteria inhibit this fusion to evade destruction.
What strategies do intracellular bacteria use once they have entered a host cell?
Intracellular bacteria either inhibit phagosome-lysosome fusion to survive, create bacterium-containing vacuoles as a protective niche, survive in the harsh conditions of the lysosome, or regulate cell death to their advantage.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in