
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
The biomedical profession's moral and ethical principles surpass boundaries and adhere to the same core concepts: respect for patient's autonomy, beneficence, non-maleficence, and justice1. Several factors about gene therapy have prompted concerns among scientists, legislators, and the general public. These include the fast progress and accessibility of gene editing, the unknowns with regards to long-term consequences, the danger and impact of unintentional and unplanned gene alterations, as well as purposeful abuse and malicious use of gene-editing technology.
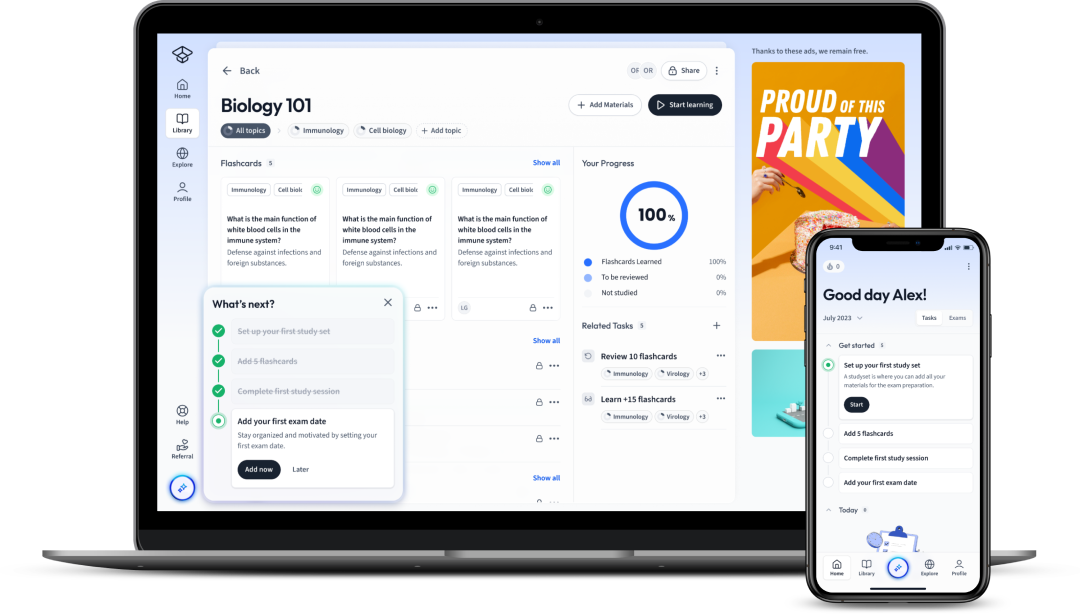
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenThe biomedical profession's moral and ethical principles surpass boundaries and adhere to the same core concepts: respect for patient's autonomy, beneficence, non-maleficence, and justice1. Several factors about gene therapy have prompted concerns among scientists, legislators, and the general public. These include the fast progress and accessibility of gene editing, the unknowns with regards to long-term consequences, the danger and impact of unintentional and unplanned gene alterations, as well as purposeful abuse and malicious use of gene-editing technology.
The introduction of cloned genes into somatic cells or altering existing genes to cure illness is referred to as gene therapy.
Since Hippocrates, "do no harm" has been a basic challenge of the medical profession. Gene therapy is no exception. Finding a therapy for severe diseases should be helpful to the patient, or at least not be any worse than the sickness itself.
Over 7,000 genetic disorders have been identified in humans that involve abnormalities in a single gene. Examples of them include cystic fibrosis, sickle cell anaemia, and haemophilia. These conditions can be very good potential candidates for gene therapy.
Risk-benefit assessment or risk/benefit analysis involves comparing the benefits that a potential treatment offers to the risks of not using the treatment, using conventional treatments, and the risk of the adverse effects that the said treatment can create. If the risks outweigh the benefits, then using the treatment would be counterproductive and not advised.
Genome editing (also known as gene editing) refers to technologies that allow scientists to alter an organism's DNA. These technologies enable the addition, removal, or modification of genetic material at specific sites in the genome.
Nevertheless, the current knowledge of gene editing is insufficient to predict the medium and long-term consequences of making specific changes in the genome. Furthermore, the impacts of gene editing can last more than one generation since parents pass on their genes to their children. Due to these concerns, gene therapy raises debate among scientists, clinicians and the general public. Some have advocated for a ban on genome-editing technologies in humans, while others believe that the benefits of this technology outweigh the hazards.
Choosing candidates for gene therapy requires certain criteria to be met. These include:
While somatic gene editing is widely regarded as a feasible treatment for severe genetic disorders and cancer, it is widely believed that modified germline cells should not be used for reproduction.
Somatic gene editing involves making alterations to the DNA of a somatic cell. A somatic cell is any biological cell in the body of a multicellular organism that is not a gamete, germ cell, or an undifferentiated stem cell.
Germline gene editing is defined as altering the genome in germline cells. These germline cells are a group of cells in a sexually reproducing multicellular organism that pass on their genetic material to their progeny. They can undergo meiosis to produce gametes.

Supporters of germline editing argue that deleting mutations in embryos inheriting a severe genetic condition will reduce the pool of mutations, benefitting humanity overall. This is true for many monogenic disorders, but others are sporadic (occurring in only one family member) or caused by chromosomal rearrangements or de novo mutations that cannot be predicted and hence cannot be rectified.
The risk-benefit analysis is a complex concept that considers factors such as the patient's age, the severity of the disease, the availability of alternative treatment, the psychosocial and economic costs of both performing and not performing the procedure, and yet unknown factors. While the risks of traditional therapies are weighed against the benefits of the patient or group of patients, the assessment of risks and benefits in gene therapy should go beyond the patient since it can affect future generations.
Furthermore, treating a known mutation does not rule out the possibility of another undiscovered mutation being present in a different gene. The targeted mutation may be masking the undiscovered mutation and preventing it from causing any noticeable signs and symptoms. But by treating the targeted mutation, the signs and symptoms of the undiscovered mutation may start to show. Therefore, people treated with gene therapy may show different side effects. This emphasizes the importance of screening for other mutations before starting gene therapy.
We don't know if a mutation that increases the risk of one chronic condition doesn't also protect against another. For instance, a change in the genome of T cells aimed at rendering resistance to HIV was discovered in 2016 to enhance vulnerability to the West Nile virus2.
The situation is much more complex in multifactorial disorders. Since these conditions may be a product of multiple dysfunctional genes or environmental elements, editing a single gene will not be sufficient for effectively treating them. And attempting to alter multiple genes brings on more controversy, since it increases the risks of side effects and unwanted mutations that can have very negative outcomes.

Multifactorial disorders are those that are not caused by dysfunction in a specific single gene and are more likely to be related to the influences of several genes and the effects of environmental factors. Schizophrenia, Alzheimer's disease, diabetes, asthma, obesity, epilepsy, and hypothyroidism are examples of multifactorial conditions.
Based on the concept of beneficence, the physician has a duty to care for the patient while minimizing the risks.
Beneficence has multiple levels concerning hereditary conditions:
When the sickness is severe, and there are not any traditional treatments that can cure or improve the symptoms, it is quite likely that a well-designed gene-editing therapy would be seen as more useful and preferable than traditional medications or the disease's natural progression.
An example of this would be spinal muscular atrophy (SMA) which affects the central and peripheral nervous system and skeletal muscles. Since no traditional medicine is effective in curing or improving the symptoms of this condition, gene therapy has been the main tool for treating SMA, and the FDA and NICE have approved a few gene therapies for clinical use.
On the other hand, using gene therapy for a flaw, such as colour blindness, which has limited effects on quality of life and allows for a reasonably normal lifetime, can have a significantly greater risk to benefit ratio, making the treatment not endorsed unless the risks are less than minimum. This is why a higher risk associated with gene-editing treatment must be evaluated against the likelihood of the illness being mild.
If the genetic condition affects several organs and systems, it is critical to collaborate in a multidisciplinary team to provide the patient and family with the finest care possible. This is particularly true for long-term follow-up after gene therapy when the physician is seeking indications of off-target or harmful consequences in addition to monitoring the progression of the primary illness.
A multidisciplinary team is a collection of health care specialists from various fields (professions such as Psychiatrists, Social Workers, and so on) who each provide unique care for the patient.
Involving the patient in the decision-making process about their diagnosis and treatment plan, which can take into consideration the health-related advantages and their beliefs and cultural values, is an essential aspect of medical care. A realistic approach would be to present the patient with a thorough and clear description of the issues, potential therapies, and recommendations, allowing them to make an informed decision.
Informed consent: If the information is supplied by a trained professional to a patient who is competent to understand and remember, make a decision, and communicate to the research or medical team, the patient's consent can be termed informed.
Regarding reproductive options and prenatal gene therapy, the family, and ultimately the mother, must make the decision.3
Genetic information can be difficult to understand for the public or even some members of the healthcare team, which is why it should be presented by a geneticist, a genetic counsellor, or another person trained in genetics to ensure that the patient correctly understands the therapeutic intervention.
For example, the genome can be portrayed as an instruction manual, with certain words misspelt or misplaced, making the text difficult to grasp; the goal of the therapy is to rectify these errors. Additional information regarding the methods used in the therapy can be included.
A patient with an untreatable serious disease may perceive any therapy as preferable, and not properly evaluate the risks. However, the hazards, potential remedies, reversibility, or alternatives should be clearly highlighted.
In the case of somatic gene-editing therapy for cancer, for example, traditional methods (chemoradiotherapy) can be presented as an option; in embryo editing for the prevention of a genetic disease that runs in the family, in vitro fertilization and preimplantation genetic diagnosis can be offered to select healthy embryos for implantation.
One of the primary concerns about genome editing in gene therapy is the possibility of it being utilized for non-medical goals, such as augmentation or eugenic activities.
Eugenics can be defined in several ways, but in general, it refers to the process of introducing specific modifications in a population's genetic composition to enhance its phenotype.
Human enhancement is most commonly associated with the genetic engineering of humans, which involves changing genetic material to create a selection advantage such as immune protection, height, muscle mass, intelligence, etc. Advanced understanding in genomics and genome editing has reignited the debate over human improvement and the ability to pick the traits of our offspring in the same way that we choose clothes in a store.
"Designer babies" is a commonly used phrase to describe human beings whose genes have been deliberately edited to offer particular qualities, such as the colour of their eyes, hair, or skin, based on their parents' preferences.
In agriculture, eugenics has long been employed to improve the quality of livestock and plants.
For animals grown for meat, the biggest muscle mass can produce much more meat than ones with less muscle. In plant agriculture, plants that produce the biggest yield are much better for farmers to grow.
Can selecting an embryo for in-vitro fertilization (IVF) from a pool of other embryos with various genetic features be described as eugenics? What about terminating a pregnancy with an afflicted embryo? Or do the family have a right to have a healthy child and express reproductive autonomy? These issues are controversial.
Some argue that a family's decision to pick a healthy embryo and eliminate one with a harmful genetic mutation is not eugenics because it is restricted to an individual or a family and will not impact a broader population. However, the patient's or their family's choice may be influenced by the availability of medical treatment and societal restraints.4
We know very little about what genes cause us to be smarter, taller, or stronger; all of these are multifactorial characteristics that come from the combination of our genome and environment. If we attempted to tweak our DNA to enhance its qualities, we would have to make several modifications at once without correctly predicting the effect.
There is a widespread agreement in the scientific community that germline editing, particularly non-medical uses, should be prohibited and that a major public consultation should take place before any application is launched. When genome editing is approved to be utilized for therapy, a suitable supervision structure should be in place to avoid it from being misused.5,6
First Name Second Name, Full title, Journal, Date
2. Beth Baker, The Ethics of Changing the Human Genome, BioScience, 2016
3. S. Hostiuc, ed., Clinical Ethics at the Crossroads of Genetic and Reproductive Technologies, 2018
4. C.J. Epstein, Is modern genetics the new eugenics? Genet Med. 2003
5. Beth Baker, The Ethics of Changing the Human Genome, BioScience, 2016
6. J.H. Wang, R. Wang, et al., Public attitudes toward gene therapy in China, Molecular Therapy-Methods & Clinical Development, 2017
Rapid advancements in genome-editing technology promise to deliver the most effective treatment option for hereditary disorders and cancer. Before recommending gene-editing therapy to a patient with a genetic disease, doctors must consider the following factors: disease type, inheritance, natural evolution, potential immediate and long-term serious complications, alternative therapies, and other associated risks.
Scientists, healthcare experts, patients, and the wider public must determine when, under what circumstances, for what conditions, and at what ages this technology should be used in the therapeutic setting to deliver the greatest benefit with the least harm.
However, the rare human results of targeted genetic modifications suggest prudence and a thorough knowledge of the processes before proceeding with any therapeutic application of genome-editing tools.
There are five main steps involved in a gene therapy plan:
Flashcards in Ethical Considerations of Gene Therapy30
Start learningWhat are the core ethical principles of biomedical ethics?
respect for patient's autonomy, beneficence, non-maleficence, and justice
What questions need to be asked when assessing the suitability of candidates for gene therapy?
The impacts of gene editing can last more than one generation
True
What factors does the risk-benefit analysis take into account?
the patient's age, the severity of the disease, the availability of alternative treatment, the psychosocial, and economic costs of both performing and not performing the procedure, as well as yet unknown factors
A change in the genome of T cells aimed at rendering resistance to the HIV virus was discovered in 2016 to enhance vulnerability to the West Nile virus
True
What are the levels of beneficence in the medical context?

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in