
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Explore the comprehensive guide to Creutzfeldt-Jakob Disease in this instructive and thorough exposition. Grounded in microbiology, you'll gain crucial insights into the nature and implications of this rare and degenerative brain disorder. The content delves into the biological relationship of the disease with biological molecules, the signs and symptoms, the different types, causes, risk factors, and the impact on life expectancy. Equip yourself with knowledge on the role of prions and learn about the stages of progression. Navigate this complex topic with ease and acquire a deeper understanding of Creutzfeldt-Jakob Disease.
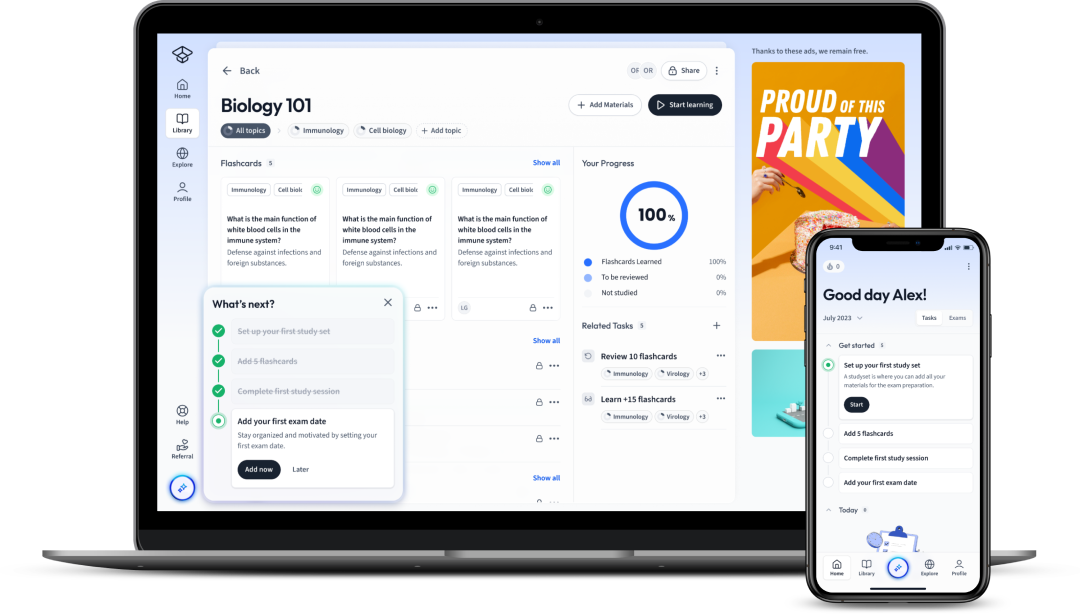
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenExplore the comprehensive guide to Creutzfeldt-Jakob Disease in this instructive and thorough exposition. Grounded in microbiology, you'll gain crucial insights into the nature and implications of this rare and degenerative brain disorder. The content delves into the biological relationship of the disease with biological molecules, the signs and symptoms, the different types, causes, risk factors, and the impact on life expectancy. Equip yourself with knowledge on the role of prions and learn about the stages of progression. Navigate this complex topic with ease and acquire a deeper understanding of Creutzfeldt-Jakob Disease.
You're probably wondering - what exactly is Creutzfeldt-Jakob Disease? Well, grab a seat and get comfortable because we're about to dive deep into the world of microbiology to explore this intriguing topic.
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, and invariably fatal brain disorder that affects about one in every one million people worldwide.
In patients with CJD, normal proteins in the brain known as prions take on an abnormal shape and accumulate, leading to neuronal death. This results in a variety of neurological symptoms such as rapidly progressive dementia, motor abnormalities, and characteristic changes on brain imaging. However, the specific reason why prions start misfolding remains a mystery.
For example, imagine a factory where every item - let's say car parts, gets moulded into the right shape for correct function. Suddenly, however, all the car parts start misshaping, and the cars produced no longer function. The same phenomenon happens in the brains of CJD patients.
At the heart of Creutzfeldt-Jakob Disease lies the problematic molecule, a prion.
Prions are naturally occurring proteins that can cause diseases when they fold in abnormal ways.
The relationship between CJD and prions can be captured in the equation below:
\[ \text{Prion Misfolding} \Rightarrow \text{Neuronal Death} \Rightarrow \text{CJD Symptoms} \]This equation might simplify things a bit, but it gets to the core of the matter. Misfolded prions lead to neurons' death, which in turn manifests as the symptoms of Creutzfeldt-Jakob Disease.
What does a diagnosis of Creutzfeldt-Jakob Disease really mean? It's not just a name; it represents a profound change in a person's life.
Understanding Creutzfeldt-Jakob Disease means recognising these implications and more. It throws light on our continuous quest to understand the mysteries of the brain and how abnormal protein folding can lead to profound changes in brain function.
Did you know? In the 1980s and 90s, a variant of CJD (vCJD) emerged as a significant public health concern when it was linked to the epidemic of bovine spongiform encephalopathy (BSE) in British cattle. Consumption of beef from infected animals was identified as the cause. This sparked an urgent need for improvements in food safety and surveillance of prion diseases.
Creutzfeldt-Jakob Disease, while rare, presents with a unique set of signs and symptoms that become progressively more severe over time. Understanding these symptoms can provide critical insights into the disease progression and contribute significantly to early diagnosis and management, although there is currently no cure.
Recognising the symptoms of Creutzfeldt-Jakob Disease is essential for early diagnosis. This disease typically manifests in three stages: early, middle and severe or late stage. Each stage has unique characteristics as the condition progresses, and the symptoms become more pronounced.
In the early stage of CJD, individuals often experience subtle cognitive and behavioural changes. These might include:
As the disease transitions into the middle stage, these symptoms become increasingly pronounced and more motor signs emerge, intensified by:
The severe or late stage is characterised by:
Recognising these symptoms early on can help in the clinical diagnosis of Creutzfeldt-Jakob Disease and ensure that supportive care is started promptly to manage symptoms and enhance patient comfort.
Note: It's important to bear in mind that these symptoms are quite common in other neurological issues. Thus, a combination of clinical features, diagnostic tests, and the rapid progression of the disease helps with CJD diagnosis.
Early detection of Creutzfeldt-Jakob Disease can be a challenge, largely due to the subtle presentation of initial symptoms. The initial signs of CJD are often non-specific and can easily be mistaken for stress, depression, or the onset of other neurodegenerative diseases.
More specifically, the following details some common early symptoms:
| Memory Disturbances | Patients might forget recent events or struggle with complex tasks. |
| Behavioural Changes | Patients might experience mood swings, apathy or withdrawal from routine activities. |
| Visual Disturbances | Patients might have difficulty with vision, such as blurring, distortion, or hallucinations. |
| Coordination Problems | Patients might exhibit unsteady gait, clumsiness, or difficulty with fine movements. |
The biology behind these early symptoms lies in the accumulation of abnormal prion proteins, mainly in the brain's cerebellum and cerebral cortex regions, regulating these functions. This accumulation causes a miscommunication between nerve cells leading to the manifestation of these symptoms.
While discussing initial symptoms, it is crucial to remember that these may vary widely among individuals due to the disease's sporadic nature. A healthcare professional's role in identifying these symptoms and referring patients for further testing is significant to ensure a detailed understanding of the disease's progression.
Creutzfeldt-Jakob Disease (CJD) is an umbrella term that encompasses a few related conditions. Each type of CJD is characterised by distinct features, presenting different symptoms, progression rates and risk factors. The core types can be categorised as: Sporadic CJD, Familial or Genetic CJD, Variably Protease-Sensitive Prionopathy (VPSPr), Iatrogenic CJD, and Variant CJD.
Variant Creutzfeldt-Jakob Disease (vCJD) is a particular form of CJD that has attracted significant public interest due to its link to bovine spongiform encephalopathy (BSE) or "mad cow disease". vCJD is believed to be caused by consuming meat from cows affected by BSE, leading to a sizeable public health crisis in the late 20th century.
The variant form, unlike other forms of CJD, often affects younger individuals, with a median age at death of 28 years compared to 68 years for classical CJD. The initial symptoms often involve psychiatric features like depression and withdrawal before advancing to more severe neurological problems. The clinical course of vCJD is more prolonged, too, with a median duration of 14 months compared to 4-5 months for the classical form.
Anatomically, large aggregates of prion protein, known as 'florid plaques', are unique to vCJD, contributing to the differing brain pathology seen in comparison to other CJD forms. These plaques cause extensive damage to the brain tissue, leading to the range of severe neurological symptoms seen in vCJD.
Understanding the nuances between different forms of CJD is key to aiding accurate diagnosis and management strategies. Here are some of the crucial differences between variant CJD (vCJD) and classical CJD.
| Aspect | Variant CJD | Classical CJD |
| Age of Onset | Young (Average age at death: 28 years) | Middle to old age (Average age at death: 68 years) |
| Initial Symptoms | Psychiatric symptoms (Depression, withdrawal) | Neurological symptoms (Memory disturbances, behavioural changes) |
| Disease Duration | Longer (Median duration: 14 months) | Shorter (Median duration: 4-5 months) |
| Cause | Consumption of BSE-infected meat | Mostly unknown (85% of cases are sporadic) |
| Brain Pathology | 'Florid plaques' formation | Spongiform changes in grey matter, without florid plaques |
Knowing these differences can not only inform clinical decisions but also assist in guiding research to unravel the mysteries of prion diseases. Despite these differences, it's crucial to remember that all forms of CJD are marked by rapid progression, severe neurological impairment, and currently, an absence of a cure.
In the quest to comprehend the causes and risk factors of Creutzfeldt-Jakob Disease (CJD), it's crucial to recognise the role of prions, the agents behind CJD. Unlike other infectious agents such as bacteria or viruses, prions are much smaller and simpler. These abnormal proteins have the ability to convert normal proteins into harmful ones, causing a domino effect of damage in the brain. The exact way that prions cause disease, and why they affect some people and not others, are active areas of research.
The primary cause behind CJD and other forms of prion disease is the misfolding of the prion protein (PrP), typically abundant in the nervous system. In their normal state, these proteins are harmless. However, under certain circumstances, the prion protein misfolds into a disease-causing form, known as PrPSc. This abnormal prion protein accumulates in brain tissue, leading to the rapid, progressive and fatal neurological symptoms associated with CJD.
Most forms of CJD are sporadic, which means they occur for no apparent reason. Around 85 percent of cases are sporadic and affect people who have no known risk factors for the disease. Still, certain genetic mutations can increase the risk, causing familial or genetic CJD. Another cause could be exposure to abnormal prion proteins, like in the case of variant CJD and iatrogenic CJD. Variant CJD is linked with eating beef contaminated with "mad cow disease", while iatrogenic CJD occurs due to inadvertent transmission of prions through certain medical procedures.
Iatrogenic means diseases caused by medical treatment. Forms of iatrogenic CJD have been associated with procedures such as cornea transplants, dura mater grafts and injections of contaminated form of human growth hormone.
Even though the causes can vary, the underlying pathogenesis involving the accumulation of abnormal prion proteins in the brain remains consistent across all types of CJD.
Prions are at the heart of what makes CJD a fascinating and challenging field of study. Prions represent a radical departure from conventional infectious agents because they lack genetic material. Composed entirely of protein, prions can still replicate and cause disease, posing a unique conundrum in biology.
Despite containing no DNA or RNA, prions cause disease by interacting with the normal prion protein, denoted as PrPC. Prions, which are a misfolded form of the prion protein (PrPSc), bind to PrPC and induce a conformational change, converting the normal protein into the disease-causing form. This process can be represented by the following equation, formatted using LaTeX:
\( \text{PrP}^{C} + \text{PrP}^{Sc} \rightarrow 2\text{PrP}^{Sc} \)
This equation describes the prion replication model where one molecule of normal prion protein (PrPC) interacts with one molecule of the abnormal prion protein (PrPSc) to produce two molecules of PrPSc. This process continues, leading to exponential growth of the abnormal prion protein and the onset of disease symptoms.
It's important to remember that prions are not destroyed by normal sterilisation methods, making them particularly dangerous. Furthermore, the lack of any nucleic acid genome means prions are not susceptible to common antiviral medications. Understanding the unique pathophysiology of prion diseases, such as CJD, is crucial to developing effective treatment strategies in the future.
To give an analogy, imagine being in a room filled with domino tiles set up in a chain. If one tile is tipped, it would knock down the next in succession, and that would hit the next, and so forth. The prion disease process is somewhat similar. The abnormal prion (PrPSc) interacts with a normal prion protein (PrPC) and causes it to misfold into the abnormal form, starting a chain reaction that gradually leads to a build-up of PrPSc, causing damage which becomes apparent as the disease symptoms.
Creutzfeldt-Jakob Disease (CJD) is a rapidly progressing condition. As an incurable neurodegenerative disorder, understanding its progression and expected life expectancy can help patients and their loved ones make informed decisions regarding care, management, and end-of-life planning.
As with many neurological disorders, CJD presents itself in distinctive stages, each marked by a progressive worsening of cognitive, emotional, and physical symptoms. These broadly encompass the early, middle, and late stages of the disease.
The early stage often manifests as subtle changes in personality, behaviour, and motor functions. Patients may experience symptoms such as memory issues, mood changes, anxiety, depression, and initial challenges with coordination and visual disturbances.
The middle stage is when the more profound neurological symptoms become apparent. Motor issues might intensify, leading to jerking movements, muscle stiffness and weakness. Cognitive decline also escalates, creating difficulties with language, comprehension, and recognising familiar faces or objects.
In the late stage, the disease continues to escalate, leading to severe mental and physical deterioration. Complete dependency on care becomes inevitable due to mobility limitations, often coupled with speech difficulties, and extreme disorientation. The end is typically marked by severe weakening of the body and a susceptibility to infections, especially pneumonia.
Another key aspect of CJD progression is the appearance of specific wave patterns on an electroencephalogram (EEG). These waveforms, known as 'periodic sharp and slow wave complexes' (PSWCs), can help diagnose CJD. The formula is presented in LaTeX format below:
\( \text{PSWCs} = \frac{\text{number of sharp waves}}{\text{duration of recording in seconds}} \times 60 \)
This formula calculates the frequency of PSWCs per minute, which is often significantly higher in people with CJD as compared to other neurological conditions. However, while the presence of PSWCs is a strong indicator of CJD, their absence does not rule out the disease, as they might not be present in the early stages or in certain types of the disease.
Life expectancy in CJD is heavily dependent on the type of CJD one has. On average, patients with sporadic or variant CJD live about a year after symptoms first appear. Nonetheless, this can range somewhere between a few months to a few years. However, people with familial CJD tend to have a slightly longer life expectancy, though it still remains significantly reduced compared to the general population.
Below is a comparison between the life expectancies of the common forms of CJD:
| Type of CJD | Average lifespan after symptoms onset |
| Sporadic CJD | ~ 1 year |
| Genetic CJD | 1-2 years |
| Variant CJD | ~ 1.5 years |
These figures underscore the severity of CJD, especially given its rapid progression. However, it is vital to remember that these are averages, and individual cases may deviate from these estimations. Many factors, such as age, overall health, and the severity of symptoms, can influence life expectancy in CJD patients.
The rapidity with which CJD advances typically leaves little time for doctors to pursue aggressive treatment plans and thus, their focus generally shifts on improving the quality of life for patients in their remaining time and offering symptomatic relief. Clinical trials and research studies are currently being conducted to explore potential therapies for CJD, though as yet, there are no approved treatments that can slow or halt progression of the disease.
Flashcards in Creutzfeldt-Jakob Disease15
Start learningWhat is Creutzfeldt-Jakob Disease (CJD)?
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, fatal brain disorder caused by misfolded prions leading to neuronal death. It results in rapidly progressive dementia, motor abnormalities, and changes on brain imaging.
What are the implications of a diagnosis of Creutzfeldt-Jakob Disease?
A diagnosis of Creutzfeldt-Jakob Disease signifies rapid progression of the disease, significant impact on quality of life due to symptoms range, and a lack of cure. It usually leads to death within a year of onset.
What is the biological relationship between Creutzfeldt-Jakob Disease and prions?
Prions are proteins that, when misfolded, lead to neuronal death and result in the symptoms of Creutzfeldt-Jakob Disease.
What are some of the early symptoms of Creutzfeldt-Jakob Disease?
The early symptoms of Creutzfeldt-Jakob Disease include memory disturbances, behavioural changes, visual disturbances, and coordination problems.
What happens as Creutzfeldt-Jakob Disease transitions into the middle stage?
As Creutzfeldt-Jakob Disease moves into the middle stage, symptoms such as severe mental impairment, speech impairment, and sudden, brief, shock-like movements known as myoclonus become more pronounced.
What characterises the severe or late stage of Creutzfeldt-Jakob Disease?
The severe or late stage of Creutzfeldt-Jakob Disease is characterised by complete immobility, muteness, inability to care for oneself, and lack of responsiveness to the environment.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in