
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Dive deep into the world of microorganisms and human diseases as you discover the ins and outs of Fatal Familial Insomnia. This rare, genetic neurodegenerative disease holds many mysteries, from its biological context to its tell-tale symptoms. This comprehensive guide takes you through an in-depth exploration of this condition, unveiling its causes, examining real-world cases and studies, and eventually discussing the available treatment options and the life expectancy of patients diagnosed with it. By shedding light on such a rare condition, you'll empower yourself with beneficial knowledge that can enhance your understanding of human genetic disorders.
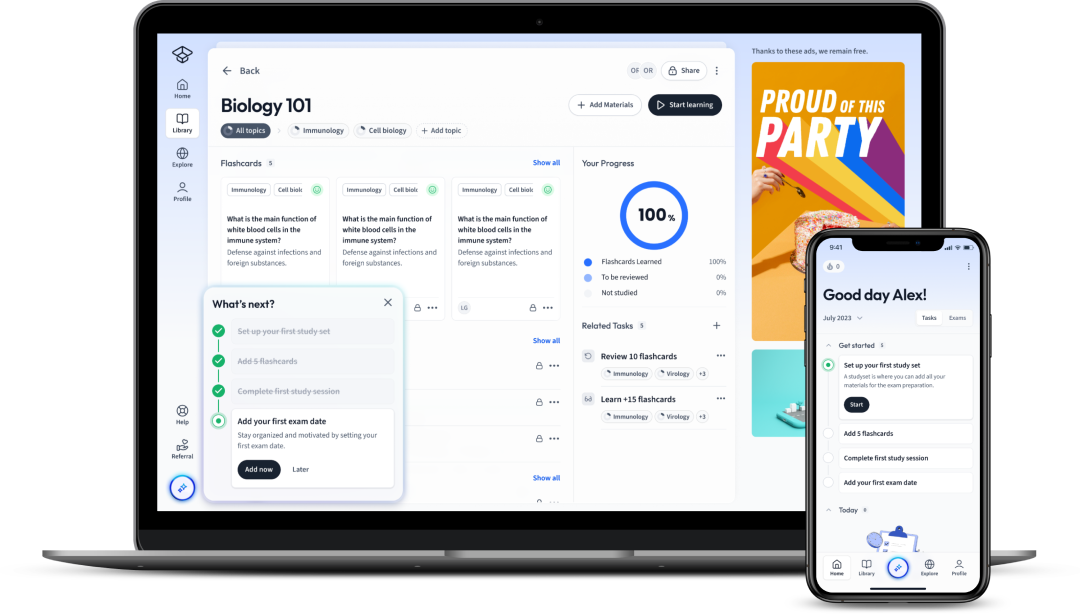
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDive deep into the world of microorganisms and human diseases as you discover the ins and outs of Fatal Familial Insomnia. This rare, genetic neurodegenerative disease holds many mysteries, from its biological context to its tell-tale symptoms. This comprehensive guide takes you through an in-depth exploration of this condition, unveiling its causes, examining real-world cases and studies, and eventually discussing the available treatment options and the life expectancy of patients diagnosed with it. By shedding light on such a rare condition, you'll empower yourself with beneficial knowledge that can enhance your understanding of human genetic disorders.
Fatal Familial Insomnia (FFI) is a rare inherited brain disorder characterised by the inability of the affected individual to sleep, which progressively worsens over time. This condition is so severe that it eventually leads to significant physical and mental deterioration and ultimately, death.
FFI is caused by a specific mutation in a gene known as PRNP (prion protein gene). This mutated gene produces an abnormal version of the prion protein which then accumulates in the brain, causing damage to the neurons. Over time, the damage intensifies, resulting in the person affected losing their ability to sleep. The condition is autosomal dominant, meaning you only need to inherit the mutated gene from one parent to develop the disease.
| Prion Protein (Normal) | PRNP Gene (Normal) |
| Mutated Prion Protein | Mutated PRNP Gene (FFI) |
While FFI affects people of all races and ages, the onset of symptoms typically starts during middle age. Despite its rarity, studying FFI is essential due to its therapeutic implications for understanding other more common neurodegenerative diseases such as Alzheimer's and Parkinson's.
The prion protein is known for its 'shape-shifting' abilities. Under normal conditions, the prion protein exists in a harmless conformation, known as PrP^C. However, the alteration caused by the mutation changes the structure of the protein to an abnormal form called PrP^Sc.
\[ \text{Harmless conformation: PrP}^C \] \[ \text{Abnormal conformation: PrP}^Sc \]An illustrative example of how prions work can be found in the game of dominos. Each prion protein is a domino piece. When one successfully 'tumbles', it induces other 'domino pieces' (other prion proteins in this case) in close proximity to also tumble, causing a cascading effect. This process is very much like the transformation from the harmless PrP^C to the harmful PrP^Sc.
The accumulation of this abnormal protein in certain areas of the brain, particularly the thalamus (a part responsible for regulating sleep), poses a significant problem. The thalamus starts to shrink, adversely impacting its function and thereby resulting in the sleep disturbances characteristic of FFI.
While this phenomenon can be theoretically modelled, the exact biochemical and biophysical processes leading to neuron damage in FFI, as in many other neurodegenerative diseases, continue to elude scientists. More research is essential in this field to improve our understanding and find a potential cure.
Fatal Familial Insomnia, as a progressive neurodegenerative disease, comes with an array of symptoms. These symptoms often begin subtly before gradually worsening, causing considerable physical and cognitive changes that can significantly affect the quality of life of the afflicted individual. It's crucial for those at risk to be well-versed with these symptoms as early detection can facilitate better management of the condition.
Fatal Familial Insomnia has some common symptoms that tend to show up in most sufferers. Chiefly, the condition earns its name from the progressive sleep disturbances it causes. However, it's important to note that these disturbances aren't the typical form of insomnia you might think of but rather an increasingly persistent inability to achieve deep or REM sleep due to damage to the thalamus.
The effects of this sleep deprivation build over time, bringing about concomitant physical and neurological symptoms that worsen as the disease progresses. These typically involve:
Medical professionals diagnose Fatal Familial Insomnia based on these symptoms, but the conclusive diagnosis often requires genetic testing to identify the presence of the mutated PRNP gene.
When Fatal Familial Insomnia first strikes, the symptoms can be quite mild, appearing like classic insomnia cases, and often misdiagnosed. Over time, the inability to sleep becomes increasingly persistent, leading to a state of near-total sleep loss.
During this initial phase, a person may also experience panic attacks and unusual phobias. As the disease progresses, more severe symptoms begin to appear.
| Persistent Insomnia | Panic Attacks | Unusual Phobias |
| Increasing Body Temperature | Rapid Weight Loss | Chronic Fatigue |
The progression of Fatal Familial Insomnia is marked by a severe worsening of symptoms. Persistent insomnia evolves into chronic sleeplessness, leading to rapid, stark weight loss and amplified physical symptoms like tremors and a lack of coordination.
The disease also exhibits neurological progression, with advanced stages causing cognitive symptoms, such as substantial memory loss and a decline in mental faculties, constituting a state of progressive dementia. There may also be hallucinations brought on by severe sleep deprivation.
Symptoms of FFI are progressive and predictable, but the onset of the disease, as well as its rate of progression, can vary from person to person. A medical professional's guide and genetic testing remain crucial for an accurate diagnosis and bracing for this condition's progression.
Fatal Familial Insomnia, while characterised by its sleep-related symptoms, is fundamentally a genetic disorder triggered by specific mutations within the prion protein gene, PRNP. PRNP plays a significant role in producing prion proteins that, under abnormal conditions, cause disruption in brain function leading to FFI.
Fatal Familial Insomnia primarily finds its roots in genetic mutation. The PRNP gene located on chromosome 20 is responsible for producing the prion protein (PrP) that naturally exists in harmless form within the body. However, a mutation within this gene alters the resulting PrP, producing an abnormal form that ultimately causes FFI. Understanding the course of these changes aids in comprehending the mechanics of Fatal Familial Insomnia.
First and foremost, the normal prion protein known as PrPC is primarily alpha-helix-rich. However, the specific mutation in the PRNP gene leads to the production of an abnormal PrPSc protein which contains a higher proportion of beta-sheets, which gives it the propensity to clump together.
\[ \text{Normal PrP (PrP}^{C}\text{)} \to \text{Abnormal PrP (PrP}^{Sc}\text{)} \]This process, illustrated in the formula above, results in the aggregation of these abnormal proteins, forming 'clusters' that are particularly damaging to brain tissues. Of particular note is the Thalamus, a section of the brain substantially affected by this protein clustering. The Thalamus regulates sleep and other crucial body functions, its deterioration hence leading to the notorious sleep disturbances of FFI.
Of note, Fatal Familial Insomnia is an autosomal dominant condition, meaning that an individual only needs to inherit one copy of the faulty PRNP gene from either parent to develop the disease.
Furthermore, another intrinsic factor in the pathogenesis of FFI is the 'species barrier', posing a challenge in research involving experimental animals. This barrier results from differences in the prion protein sequence between species, leading to a varying degree of susceptibility to prion diseases.
As with many genetic diseases, unravelling the thread of the underlying causation starts with the genotype - the specific genetic makeup of an individual pertaining to a particular trait or set of traits. The genotype involved in FFI is rooted in the change or mutation within the PRNP gene.
The mutation involved in Fatal Familial Insomnia is a single nucleotide polymorphism, specifically a missense mutation. This type of mutation is one where one base substitution alters the sequence of amino acids in the protein produced. In the case of FFI, this translates into the mutation from the normal Methionine (Met) to Valine (Val) at codon 129.
\[ \text{Normal Methionine (Met)} \to \text{Abnormal Valine (Val) at codon 129} \]The consequences of this mutation, while subtle at the molecular level, are profound at the physiological level, transforming the usually benign PrP into its pathogenic form, PrP^Sc. As this form aggregates and impairs cellular function, it drives the onset and progression of FFI.
It's essential to stress that this is an autosomal dominant condition, meaning that inheritance of just one copy of the mutated PRNP gene is enough for the disease to manifest. This essentially makes each child of an FFI-infected parent have a 50% chance of inheriting the disease.
Finally, it's also crucial to keep in mind that while the Met129Val mutation and subsequent PrP^Sc formation are central to FFI, not everyone with this mutation will necessarily develop FFI. Certain environmental triggers and other still-unknown genetic factors can play a role in disease onset, rendering its predictability complex and challenging.
In the quest to understand Fatal Familial Insomnia better, it's invaluable to examine real-life situations where individuals have contended with this disease and the various studies centred on this rare condition.
Fatal Familial Insomnia is an exceedingly rare condition, with fewer than 60 families reported across the globe known to carry the genetic mutation. It's recognised as a prion disease, a category of illness whereby prion proteins misfold and aggregate, giving rise to progressive neurodegenerative symptoms. One of the most extensively quoted cases of FFI is that of Silvano, an Italian man meticulously documented during his encounter with FFI.
Silvano’s exceptional case was first documented in the late 1980s by research physicians Lugaresi and Montagna in Bologna, Italy. His story exemplified the onset and progression of Fatal Familial Insomnia.
Silvano's family background further confirmed the diagnosis of FFI. A majority of his family members had succumbed to similar symptoms, causing them to suffer from sleep disorders and eventually pass away. DNA analysis from Silvano's autopsy revealed the causative mutation in the PRNP gene.
Autopsy studies of Silvano gave researchers a deeper understanding of FFI's impact on the brain, specifically the significant atrophy to the thalamus and inferior olives, reflecting their substantial role in sleep regulation.
Individual cases, as rare as they are, offer invaluable insight into the understanding of FFI. That detailed account helps in shedding light on the onset, progression and eventual outcome of the disease, allowing us to get closer to better management and, hopefully, a definitive cure.
| Initial Symptoms | Chronic Insomnia and Fatigue |
| Progression | Agitation, High Blood Pressure, Rapid Cognitive Decline |
| Genetic Confirmation | PRNP Mutation |
| Physiological Outcome | Atrophy to the Thalamus and Inferior Olives |
Over the years, the understanding of Fatal Familial Insomnia has improved immensely, thanks to numerous research studies. These studies range from exploring the genetic basis of FFI, unravelling its unique prion pathology, to the quest for potential therapeutic strategies.
One landmark study in this field was the investigation conducted by Lugaresi and Montagna, who discovered FFI in the late 1980s. In the extensive family study, they identified the condition as an autosomal dominant disorder. The researchers noted that family members presenting FFI symptoms carried the same point mutation at codon 178 of the PRNP gene, proving the causative role of this mutation in FFI.
\[ \text{Normal PRNP Gene} \to \text{Mutation at Codon 178} \]As highlighted above, this discovery triggered a plethora of new investigations into this unusual prion illness.
Interestingly, not all individuals with the mutation at codon 178 present FFI. Some individuals instead develop a condition known as Creutzfeldt–Jakob disease. The difference in disease manifestation depends on a polymorphism at codon 129 of the PRNP gene, reflecting the genetic complexity behind these conditions.
In the attempt to understand the pathogenesis and catalytic processes of FFI, various in vitro and animal model-based studies were undertaken. An important finding was the formation of the abnormal prion protein (PrPSc) mainly in the thalamus, leading to severe neurodegeneration in this area.
In addition to the genetic and pathological perspectives, research focusing on possible treatments has provided hope. Therapeutic approaches currently under consideration include:
Though the described studies have laid a solid foundation for understanding FFI, continual research is required. The rarity of this disease makes further study challenging but important. Acknowledging the efforts of scientists and researchers in exploring this disease not only enhances our apprehension of Fatal Familial Insomnia but also appeases the hopes of a sure remedy in the foreseeable future.
Fatal Familial Insomnia (FFI) is a daunting diagnosis, but it's crucial to explore the current treatment options and what they indicate for the life expectancy of individuals living with this condition.
As it stands, there is no definitive cure for Fatal Familial Insomnia, with most treatments being focused on symptomatic relief and improving the quality of life of the diagnosed individuals.
Treatment predominantly involves managing sleep disturbances, the hallmark symptom of FFI. Sedatives like clonazepam and zolpidem are often given to increase sleep duration. However, these can only counteract the symptoms to a degree and lose effectiveness over time as sleep disturbances progress.
Another approach lies in targeting the pathogenic prion protein (PrPSc) directly. Efforts are being done towards developing anti-prion compounds that could prevent the formation of PrPSc from the normal cellular prion protein (PrPC).
\[ \text{Normal PrP (PrP}^{C}\text{)} \nrightarrow \text{Abnormal PrP (PrP}^{Sc}\text{)} \]The formula above illustrates the desired effect of an anti-prion drug. A few notable compounds under study include quinacrine, an antimalarial drug and doxycycline, an antibiotic, both with anti-prion properties in some research settings.
Immunotherapeutic strategies are also being explored. These methods rely on inducing the body's immune system to negate the effects of PrPSc, thus slowing down disease progression.
It's noteworthy that all the described treatment options are still experimental and require further long-term studies to demonstrate their efficacy and safety fully. The rareness of FFI complicates human trials, and hence many of the promising treatments are primarily tested on animal models or in vitro cells.
The treatment of Fatal Familial Insomnia faces multiple obstacles, predominantly due to the rarity of the disease, the intricacy of its pathogenesis, and the 'species barrier' impeding animal studies.
Creating effective treatment protocols is a meticulous process, often taking years to attain approval. For rare diseases such as FFI, getting a sizeable sample of patients for trials is a significant challenge; as fewer the patients, the slower the progress of clinical trials.
Moreover, the complex pathogenesis of FFI adds another level of difficulty. The subtlety of the prion conversion mechanism and the specific neural structures it affects, particularly the thalamus, can make it challenging for potential therapies to target the right areas without disrupting normal biological processes.
Another hurdle comes with the 'species barrier', which poses challenges when conducting trials on animal models. This barrier is due to differences in prion protein sequences between species, affecting the transmission and manifestation of prion diseases.
Exploring treatments for FFI is thus a double-edged sword, one that promises hope for afflicted patients but also presents significant scientific challenges. However, the diligent efforts of the scientific community continue to bring us closer to innovative therapeutic strategies.
Fatal Familial Insomnia, given its progressive and currently incurable nature, understandably associates with a reduced life expectancy. On average, survival post-onset is 18 months, with a range between 7-36 months reported. The short-lived course from diagnosis to demise is primarily due to the rapid and unyielding progression of the disease.
Nonetheless, it's essential to remember that although prognosis is generally poor, life expectancy can be individual-dependent, facing influences from various factors such as the time of onset, the rapidity of disease progression, and the efficacy of symptom management.
Furthermore, a key determinant in both disease progression and life expectancy is the Met/Val polymorphism at codon 129 of the PRNP gene. A recent study has shown that MM individuals (methionine homozygous at codon 129) tend to have a more rapid disease course and hence a lower life expectancy compared to MV individuals (methionine/valine heterozygous at codon 129).
\[ \text{Met/Met (MM individuals)} \to \text{Rapid Disease Course and Lower Life Expectancy} \] \[ \text{Met/Val (MV individuals)} \to \text{Relatively Slower Disease Course and Slightly Higher Life Expectancy} \]These variations tell us that, as bleak as the prognosis may seem, there are nuances in disease manifestation and progression that could influence survival rates. A more patient-specific picture emerges - rather than a uniform outcome, presenting a more personalised narrative of the disease.
Aiding this, the continually evolving understanding of the genetic interplay and disease mechanism of FFI holds a glimmer of hope for improved management strategies and a higher quality of life for individuals grappling with the disease. It's a testament to the power of ongoing research and scientific discovery.
Flashcards in Fatal Familial Insomnia15
Start learningWhat is Fatal Familial Insomnia (FFI)?
FFI is a rare inherited brain disorder characterised by progressive insomnia, ultimately leading to physical and mental deterioration and death. It's caused by a mutation in the PRNP (prion protein gene).
What is the role of the mutant PRNP gene in Fatal Familial Insomnia?
The mutated PRNP gene produces an abnormal prion protein that accumulates in the brain, damaging neurons. Over time, this damages the ability to sleep, as the damage intensifies.
How is the onset and progression of Fatal Familial Insomnia(FFI) typically characterised?
Symptoms generally start in middle age, with early signs including insomnia, lack of appetite, and behaviour changes. As FFI progresses, physical deterioration, dementia, and severe sleep deprivation occur. The disease usually lasts 7-18 months.
What is the typical symptom that earns Fatal Familial Insomnia its name?
It's the progressive sleep disturbances causing a persistent inability to achieve deep or REM sleep due to damage to the thalamus.
What are the typical physical and neurological symptoms of Fatal Familial Insomnia?
The symptoms include persistent insomnia, rapid weight loss, high body temperature, increased heart rate, excessive sweating, loss of coordination, and progressive dementia.
What are some initial symptoms of Fatal Familial Insomnia?
The initial symptoms can appear as classic insomnia, along with panic attacks, unusual phobias, increased body temperature, rapid weight loss, and chronic fatigue.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in