
StudySmarter - The all-in-one study app.
4.8 • +11k Ratings
More than 3 Million Downloads
Free
Americas
Europe
Reproductive hormones, also known as sex hormones, are steroid hormones that play important roles in the development and maintenance of sexual characteristics, fertility, pregnancy, and menstruation.
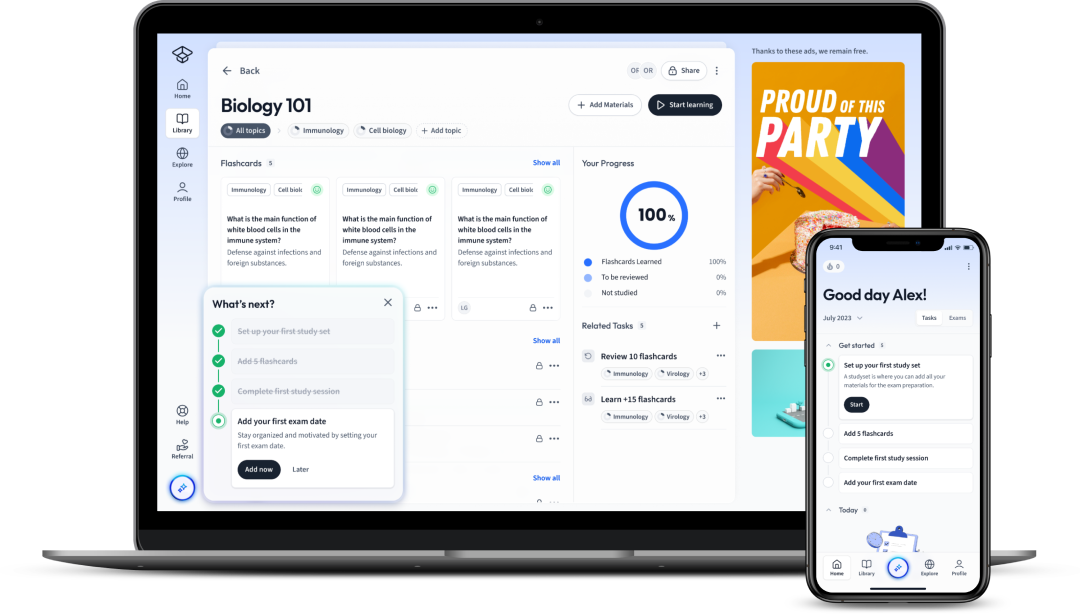
Explore our app and discover over 50 million learning materials for free.


























Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenFSH and LH stimulate the ovaries to produce mature gametes, as well as to synthesize and secrete oestrogen, the main female reproductive hormone. Women have two ovaries on either side of the uterus. The tubes that connect the ovaries to the uterus are called fallopian tubes or uterine tubes.
The levels of LH, FSH, oestrogen and progesterone in the bloodstream go through a cycle every month called the menstrual cycle. The first menstrual period happens between the ages of 11 and 15 and continues to recur every month until the beginning of menopause between the ages of 45 and 55. Each cycle normally lasts an average of 28 days (21-35 days).
The menstrual cycle refers to a monthly cycle of natural changes that occur in the female reproductive system. These changes are necessary for the production of an egg cell every month, as well as for preparing the uterus for pregnancy.
The menstrual cycle is controlled by feedback systems:
Moderate levels of oestrogen have a negative feedback effect on the HPG axis, lowering the amounts of LH and FSH released to return the oestrogen back to baseline levels. High levels of oestrogen in the presence of progesterone also have negative feedback on the HPG axis. However, high oestrogen levels without progesterone exert a positive feedback effect on the HPG axis, causing more LH and FSH to be released.
A positive feedback system, unlike negative feedback systems, amplify stimuli instead of reversing homeostatic disturbances!
The events that transpire during the menstrual cycle can be described in the context of two separate cycles, the ovarian and the uterine cycles.
The ovarian cycle consists of two phases. The follicular phase, and the luteal phase. Ovulation occurs between these two phases. It marks the end of the follicular phase and the start of the luteal phase. The follicular phase marks the beginning of a new cycle as follicles begin to mature and prepare to release an oocyte.
An ovarian follicle is a group of cells found in the ovaries that surround an egg cell and secrete hormones that regulate the menstrual cycle. Women have roughly 200,000 to 300,000 follicles at the time of puberty, each with the capacity to produce a mature egg cell for fertilization upon ovulation, meaning the release of an egg from the ovaries.
The oocyte is another term for a mature egg cell that is released every month from the ovaries.
There is minimal FSH, LH, and oestrogen in the blood at the start of a new cycle, so many follicles begin to grow independently of these hormones. Because oestrogen levels are low, there is little negative feedback acting on the HPG axis, leading to an increase in FSH and LH levels. These increase the follicle's growth and the production of oestrogen. During each menstrual cycle, only one dominant follicle can continue to grow and be released. As oestrogen levels rise to moderate levels, negative feedback decreases FSH levels, allowing just the dominant follicle to survive, which is now capable to grow independently of FSH. Follicular oestrogen gradually rises and because there is minimal progesterone in the system at this time, it exerts positive feedback on the HPG axis, triggering an upsurge in LH levels. The follicle releases the mature oocyte into the fallopian tube in response to the LH surge. This process is called ovulation. For around 24 hours, the oocyte remains viable for fertilization.
Following ovulation in the luteal phase, the remnant of the ruptured follicle becomes the corpus luteum and continues to secrete oestrogen and, for the first time, progesterone. Oestrogen in presence of progesterone exerts negative feedback on the HPG axis which lowers the LH and FSH levels to prevent the formation of any new follicles in the ovaries. Oestrogen and progesterone also maintain suitable conditions for fertilisation of the oocyte and implantation.
The uterine cycle describes the events that occur inside the uterus during the menstrual cycle, and it consists of three phases: menstruation, the proliferative phase, and the secretory phase.
Check out the Menstrual Cycle Hormones article to learn more!
The female reproductive hormone cycles outlined above are summarized in the graph below.
Exogenous hormones can be used in certain scenarios for therapeutic purposes, like Hormone replacement therapy (HRT) or Transgender hormone therapy (THT).
Hormone replacement therapy (HRT) is an effective treatment for the symptoms of menopause. HRT can also help with other long-term health issues connected with menopause, including lowering the risk of osteoporosis, cardiovascular disease, and stroke. The goal of HRT is to supplement the reduced hormone levels caused by menopause.
When the ovaries cease producing eggs, menopause has started. The hormones oestrogen and progesterone are lowered in the blood as a result of menopause. In addition to subfertility, menopause can cause symptoms such as hot flushes, dryness of the vagina and weakening of the bones. HRT works by replenishing these hormones to some degree to lower menopausal symptoms and health concerns.
Transgender hormone therapy (THT) is a type of hormone therapy in which sex hormones and other pharmacological drugs are given to transgender people to match their secondary sexual traits more closely with the gender they identify themselves with. This sort of hormone therapy is classified into two groups based on whether the target of the treatment is masculinization or feminization:
Reproductive hormones, also known as sex hormones, are steroids hormones that play important roles in the development and maintenance of sexual characteristics, fertility, pregnancy, and menstruation.
Moderate levels of oestrogen have a negative feedback effect on the HPG axis, lowering the amounts of LH and FSH released in order to return the oestrogen back to baseline levels. High levels of oestrogen in the presence of progesterone also have negative feedback on the HPG axis.
However, high oestrogen levels in the absence of progesterone exert a positive feedback effect on the HPG axis, causing more LH and FSH to be released.
Oestrogen is the main female reproductive hormone.
Testosterone is the main male reproductive hormone.
Menstruation, follicular phase, ovulation, and luteal phase
LH, and FSH from the anterior pituitary. Oestrogen and progesterone from the ovaries.
FSH and LH stimulate the ovaries to produce mature gametes, as well as to synthesize and secrete oestrogen. High levels of oestrogen exerts positive feedback on the HPG axis causing a surge in LH levels which results in ovulation. Oestrogen also promotes growth of breast tissue and makes the uterine environment suitable for fertilization. Progesterone is released after ovulation, the luteal phase. To prevent polyspermy, progesterone make the cervical environment less suitable for sperms to enter.
The menstrual cycle is controlled by feedback systems:
Moderate levels of oestrogen have a negative feedback effect on the HPG axis, lowering the amounts of LH and FSH released to return the oestrogen back to baseline levels. High levels of oestrogen in the presence of progesterone also have negative feedback on the HPG axis. However, high oestrogen levels without progesterone exert a positive feedback effect on the HPG axis, causing more LH and FSH to be released.
There is minimal FSH, LH, and oestrogen in the blood at the start of a new cycle. Because oestrogen levels are low, there is little negative feedback acting on the HPG axis, leading to a gradual increase in FSH and LH levels. These increase the follicle's growth and the production of oestrogen. Follicular oestrogen gradually rises when it reaches high levels, it exerts positive feedback on the HPG axis, triggering an upsurge in LH levels and leading to ovulation. After ovulation, the remnant of the primary follicle, now called the corpus luteum, releases both oestrogen and progesterone.
Flashcards in Reproductive Hormones70
Start learningWhat gland secretes gonadotrophin-releasing hormone (GnRH)?
The hypothalamus
What hormones are released from the anterior pituitary in response to GnRH?
LH and FSH
What is the role of LH in the male body?
LH stimulates special cells in the testes to produce testosterone, the main male sex steroid hormone.
What does testosterone do?
Testosterone has numerous roles in the body. It stimulates spermatogenesis in the testes and is essential for maintaning libido. Other actions of testosterone include development of secondary sexual characteristics through puberty (e.g. pubic and facial hair), growth of external genitalia, as well as deepening of the voice.
Testosterone also has anabolic effects and stimulates the growth of bone and muscle.
What is the role of FSH in the male body?
FSH targets another series of special cells in the testes and drives spermatogenesis in the testes.
what is the menstrual cycle?
The menstrual cycle refers to a monthly cycle of natural changes that occur in the female reproductive system. These changes are necessary for the production of an egg cell every month as well as for preparing the uterus for pregnancy.

Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place


Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in